Nigeria is currently one of several countries responding to the coronavirus disease (COVID-19) pandemic. The country has traversed through all four phases of transmission categorisation from “no case to single case to cluster of cases and currently, the community transmission phaseâ€. Through all these phases, the Nigeria Centre for Disease Control (NCDC) has continued to lead the national public health response and provide evidence-based guidelines and protocols for the response, in line with the global best practices.
Being a densely populated country with about 200 million people across 774 Local Government Areas (LGAs), the susceptibility to a virus such as SARS-CoV-2 is high. In addition to other socio-economic factors, this has significantly contributed to the ongoing community transmission in the country.
To address this, the NCDC has revised the national contact tracing strategy in line with evolving knowledge of the disease and as part of continuous engagement with the states, is supporting the implementation of this strategy at the subnational level.
On the 17th of June, 2017, the national COVID-19 Emergency Operations Centre (EOC) convened a virtual meeting with relevant stakeholders in various states. This was an interactive session with State Epidemiologists, State Disease Surveillance and Notification Officers (DSNOs), representatives of the World Health Organization (WHO) as well as United Nations Children Fund (UNICEF). The objective was to discuss strategies for increasing case detection; scaling-up contact tracing; increasing contact to case ratio and so on. The meeting also provided a unique opportunity to discuss identified challenges and how partners can work with states to address these gaps.
1. Stigmatisation and misinformation affecting surveillance activities in many states
2. Inadequate understanding of the guidelines on contact tracing and strategies for scale up of case finding and sample collection
The general consensus was the need for intensive risk communication and community engagement (RCCE), psychosocial support for suspected cases; engagement of religious/community leaders; increased resources mobilisation for contact tracing and other surveillance activities; and decentralisation of surveillance and sample collection activities to the LGAs.
As we continue to join forces in the fight against COVID-19 in Nigeria, we urge our state colleagues to prioritise contact tracing activities and leverage existing partners’ support and resources. The NCDC remains committed to supporting states to enhance their response to COVID-19.
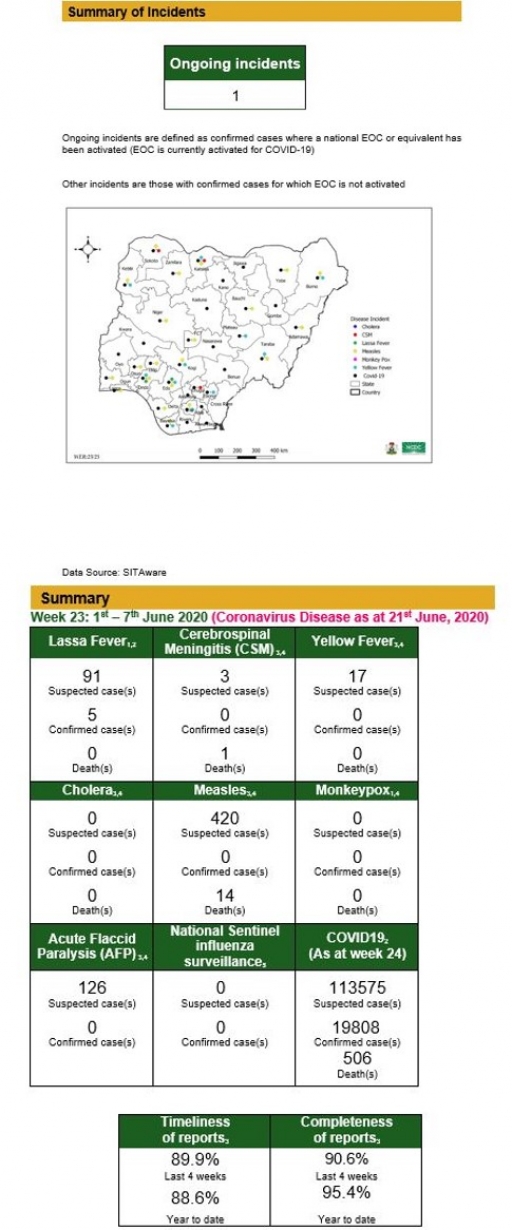
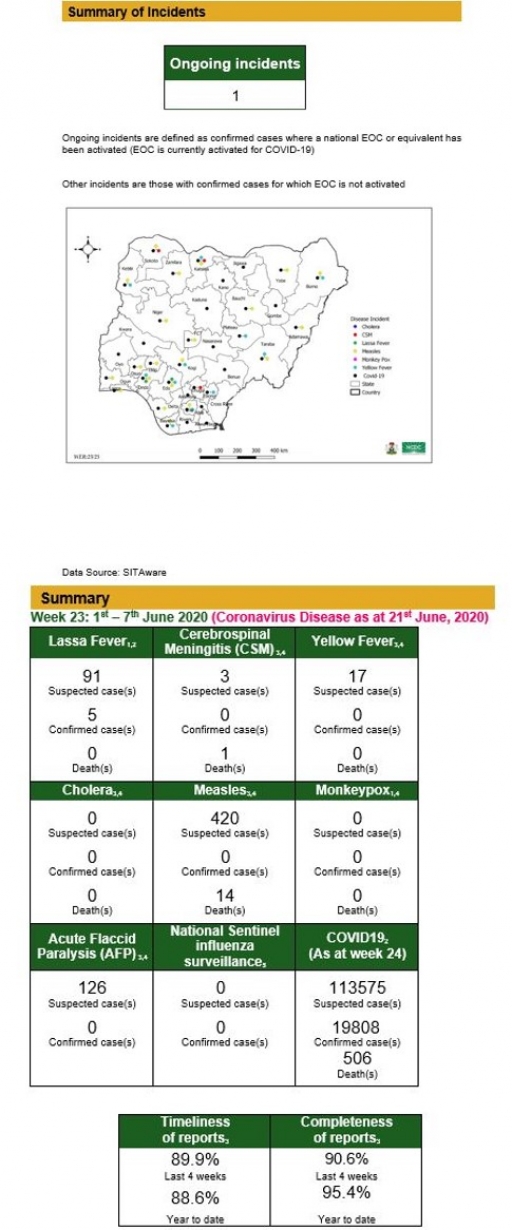
Summary of Incidents
Notes
1. Information for this disease was retrieved from the Technical Working Group and Situation Reports
2. Case Fatality Rate (CFR) for this disease is reported for confirmed cases only
3. Information for this disease was retrieved from IDSR 002 data
4. CFR for this disease is reported for total cases i.e. suspected + confirmed
5. Information for sentinel influenza was retrieved from the laboratory
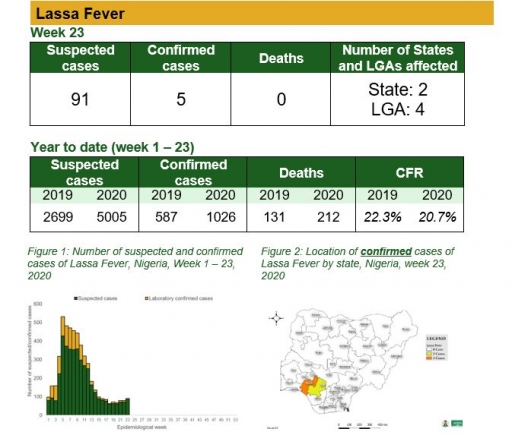
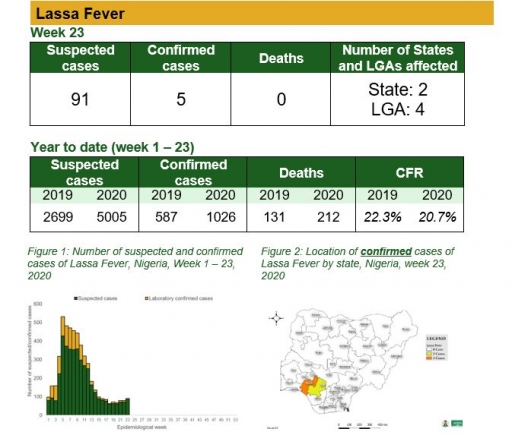
Lassa Fever
Key points
• There were 91 suspected cases, five laboratory confirmed cases and no death was recorded from four LGAs in two states
Actions
To date:
• National Lassa fever multi-partner, multi-sectoral Technical Working Group (TWG) continues to coordinate the response activities at all levels
Planned:
• Continue resource mobilisation
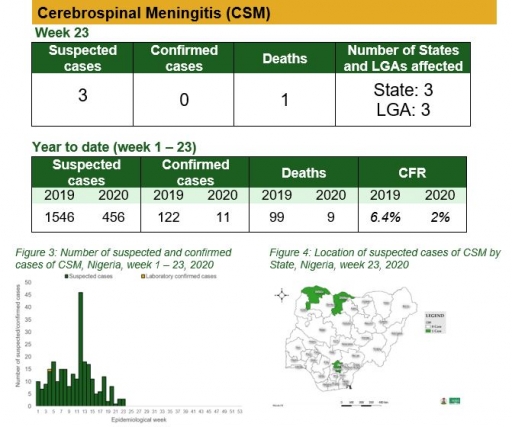
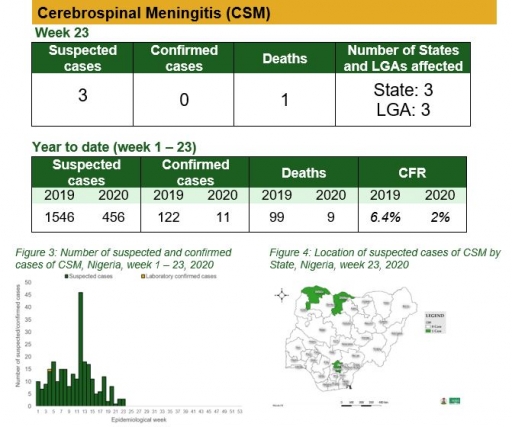
Cerebrospinal Meningitis (CSM)
Key points
There were three suspected cases of Cerebrospinal Meningitis (CSM) reported from three LGAs in three states (Enugu – 1, Katsina – 1 & Sokoto – 1). None was laboratory confirmed and one death was recorded
Actions
To date:
• National CSM TWG meets weekly to review reports from states and plan appropriately
• Enhanced surveillance in all states
Planned:
• Continue harmonisation of the national line list and SORMAS data
• Continue to ensure that states reporting cases send their line lists and collect CSM samples
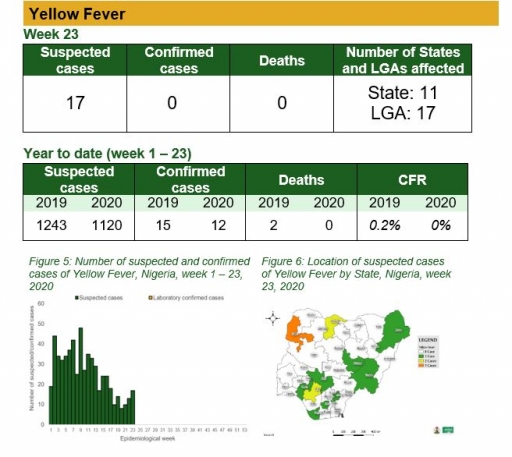
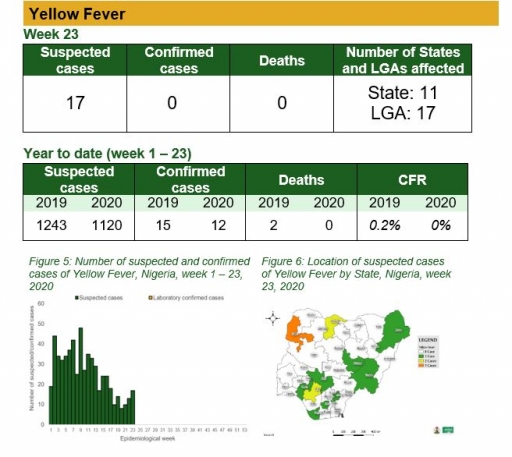
Yellow Fever
Key points
• There were 17 suspected cases of Yellow Fever (YF) reported from 17 LGAs in 11 states. None was laboratory confirmed and no death was recorded
Actions
To date:
• National multiagency YF Technical Working Group (TWG) is coordinating response activities
Planned:
• Surveillance and laboratory data harmonisation are ongoing
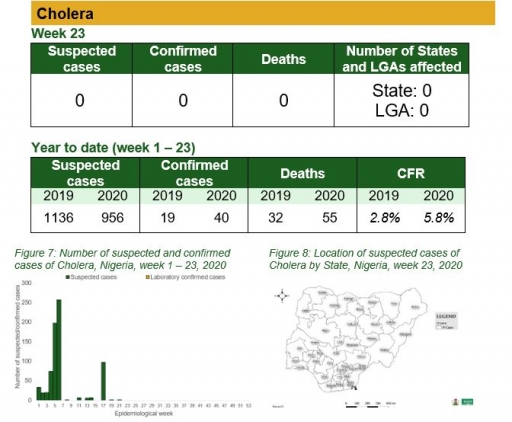
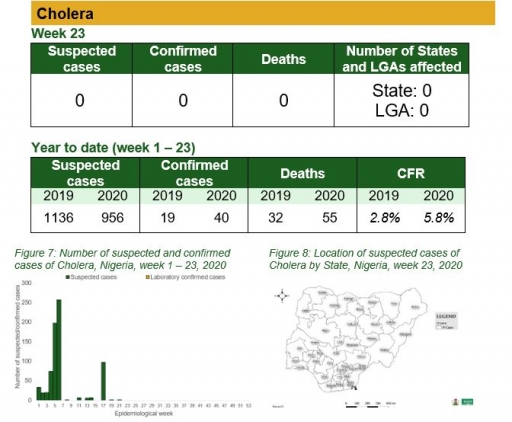
Cholera
Key points
• There was no case of cholera reported this week
Actions
To date
• National Cholera Multi-sectoral Technical Working Group (TWG) is monitoring all states and supporting already affected states
Planned:
• Continue follow up and monitoring of non-reporting states
• Continue harmonisation of the national line list and SORMAS data
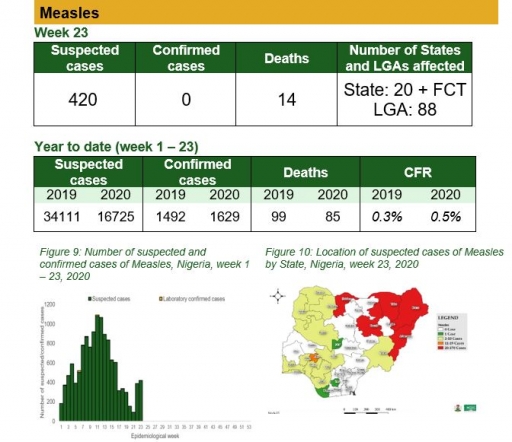
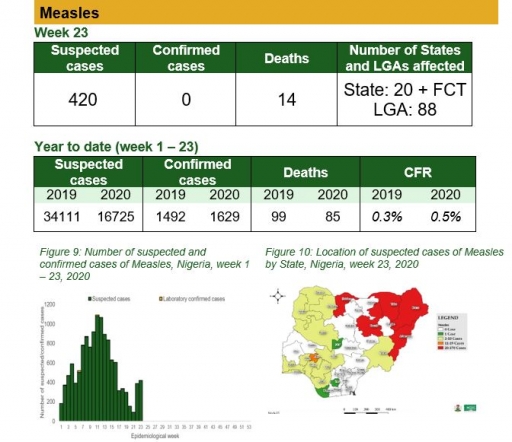
Measles
Key points
• There were 420 suspected cases of measles reported from 88 LGAs in 20 states and FCT. None was laboratory confirmed and 14 deaths were recorded
Actions
To date
• National Measles TWG is closely monitoring measles surveillance data and providing feedback to relevant agencies and development partners
• Weekly surveillance and laboratory data harmonisation ongoing
Planned:
• Monthly measles surveillance data review
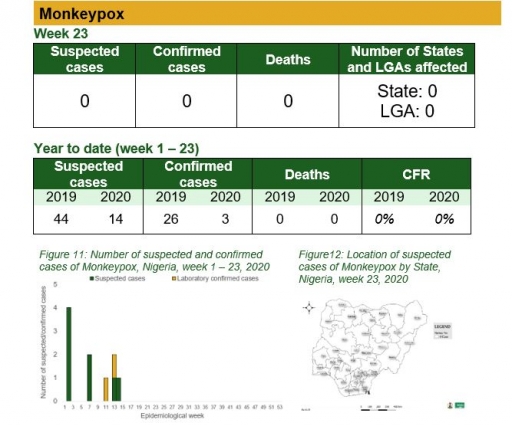
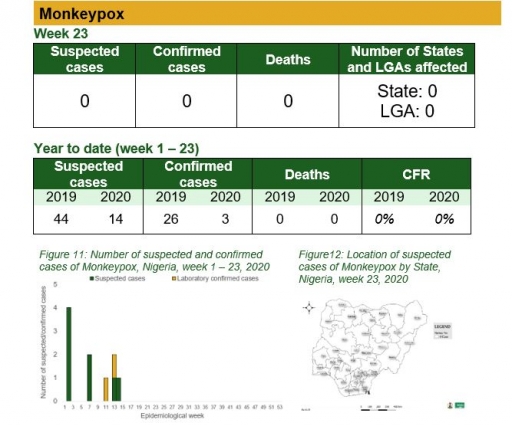
Monkeypox
Key points
• There was no case of monkeypox reported this week
Actions
To date
• National Monkeypox Technical Working Group (TWG) is monitoring activities in all states
Planned:
• Enhance surveillance for monkeypox in high burden states
• Continue harmonisation of the national line list and SORMAS data
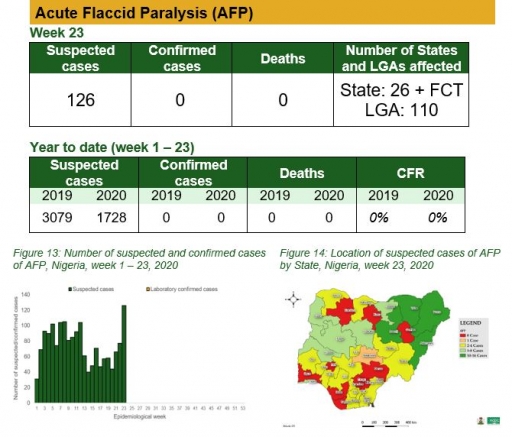
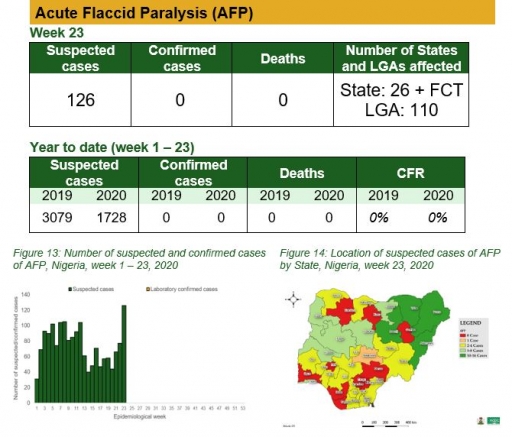
Acute Flaccid Paralysis (AFP)
Key points
• There were 126 suspected cases of AFP reported from 110 LGAs in 26 states and FCT. None was laboratory confirmed and no death was recorded
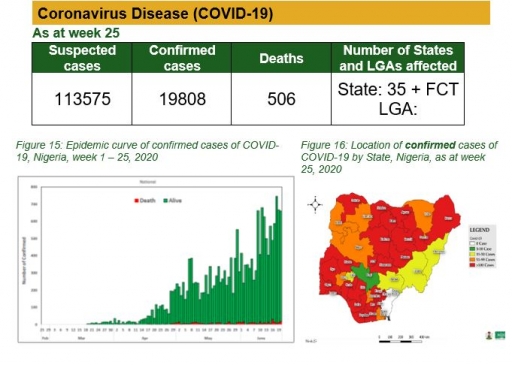
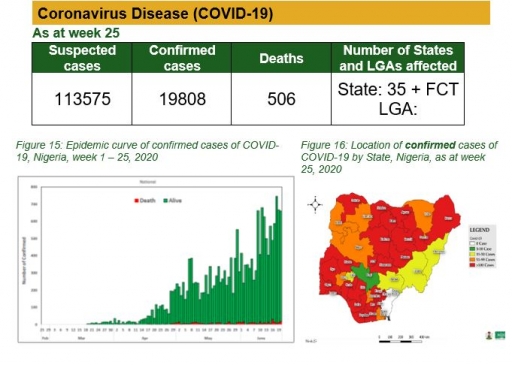
Coronavirus (COVID-19)
Actions
To date:
• National COVID-19 multi-partner Emergency Operations Centre (EOC) continues to coordinate response activities across states
• A total of 37 National Rapid Response Teams have been deployed and continues to support affected states
• Guideline for worship places launched and circulated to religious leaders and the public
• Deployment of response teams to support Port Health Services (PHS) to capture passenger information electronically into SORMAS in Lagos and Abuja airports
• Developed new graphics for COVID-19 symptoms and guidelines on re-opening of religious centres
Planned:
• Continue to engage states to discuss Contact Tracing approach and Standard Operating Procedures (SOP)
• Deployment of response teams to support Port Health Services (PHS) to capture passenger information electronically into SORMAS in Lagos and Abuja airports
• Operationalisation of COVID-19 testing in GeneXpert sites
• Deployment of mortality audit teams to states
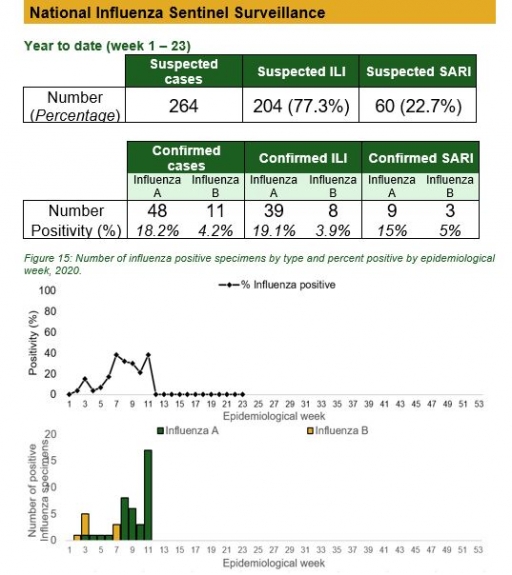
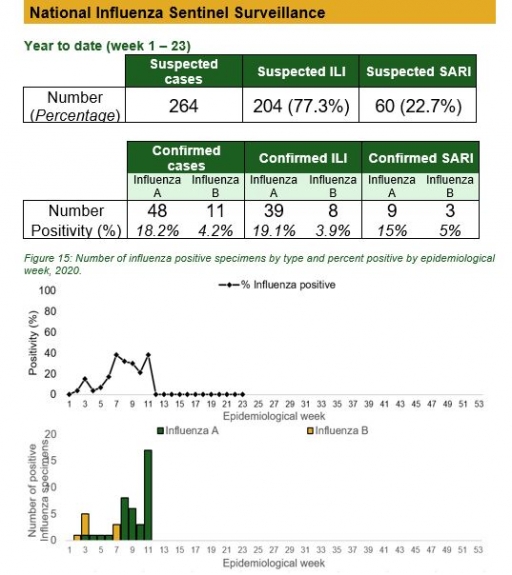
National Influenza Sentinel Surveillance
Key points
• The subtypes A seasonal H3, 2009A/H1N1 and A/not subtyped account for 0 (0.0%), 2 (9.5%) and 19 (90.5%) of the total influenza A positive sample respectively. The subtypes B VICTORIA, B Not subtyped and B Yamagata account for 0 (0.0%), 8 (100%) and 0 (0.0%) of the total influenza B positive samples respectively.
• The percentage influenza positive was highest in week 10 with 40%.
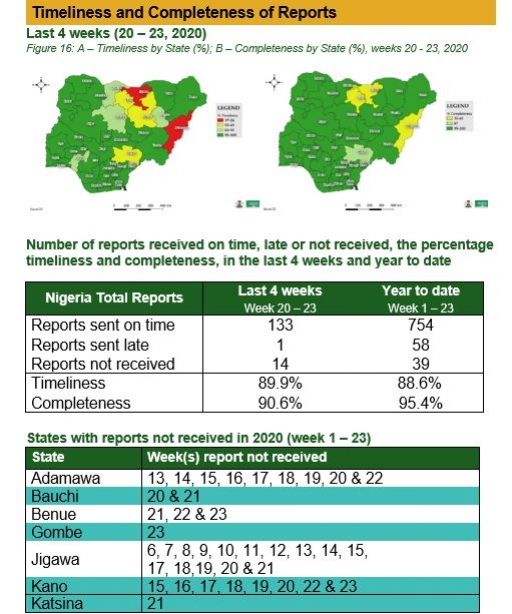
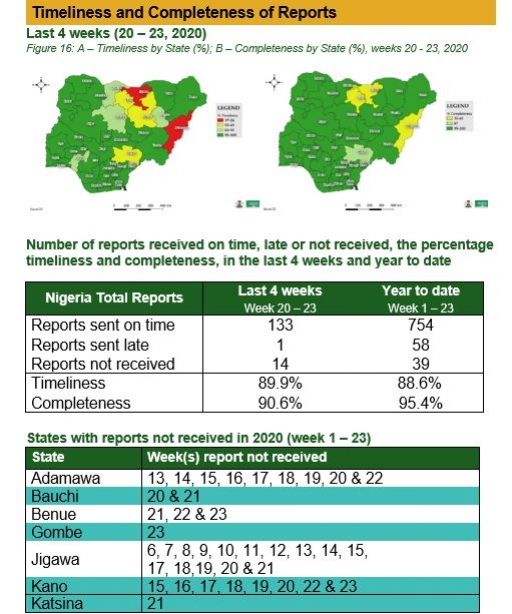
Timeliness and Completeness of Reports
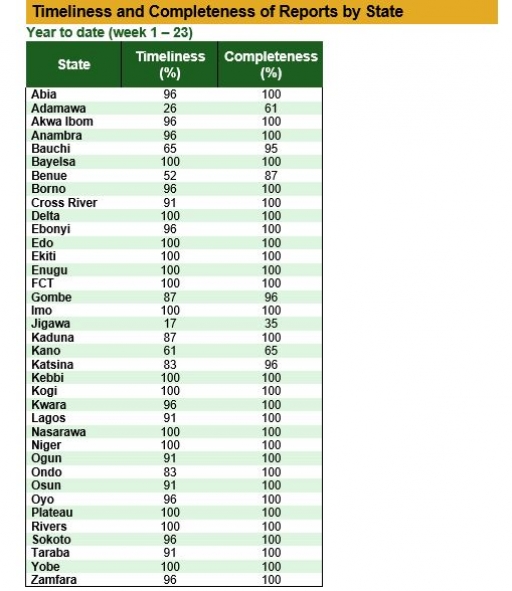
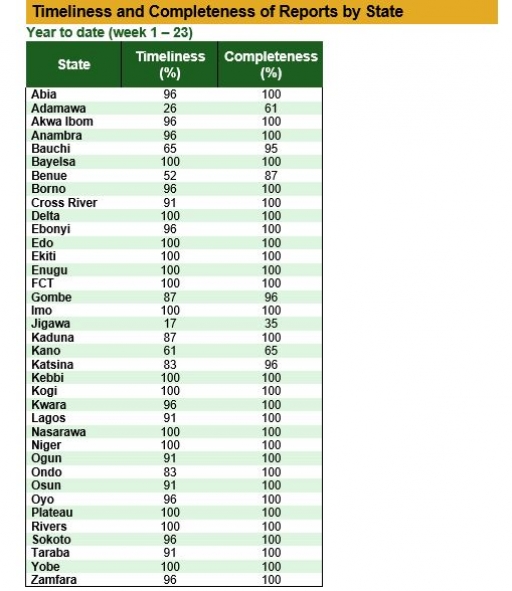
Timeliness and Completeness of Reports by State


 Toll Free Number: 6232
Toll Free Number: 6232 Whatsapp: +234 708 711 0839
Whatsapp: +234 708 711 0839 SMS Number: +234 809 955 5577
SMS Number: +234 809 955 5577 