Nigeria usually experiences outbreaks of Cholera during the rainy season. These outbreaks usually span from May up until September or October yearly. During these months, the country records high rainfalls, sometimes leading to an overflow of sewage systems and subsequent breakdown in overall hygiene standards. Furthermore, poor access to potable water and crowded living conditions are highlighted as contributory factors to the start and spread of a cholera outbreak.
In the Epi-week ending 11th June 2017, the Nigeria Centre for Disease Control (NCDC), through its event-based surveillance system received rumours of 12 deaths of Cholera in Kwara State. Initial rumour verification was carried out and a team was dispatched immediately for a full investigation and containment of the outbreak. Preliminary findings revealed a total of 1,178 suspects with 9 deaths across 4 Local Government Areas (LGAs) in Kwara State, with a CFR of 0.76% as at 14th June, 2017. Seven cases have been laboratory confirmed by culture. Affected cases have commenced treatment. Trainings on case management and infection, prevention and control are being carried out for clinicians and health care workers. Community sensitization is ongoing across the state. The Kwara State Government through the Ministry of Health is in the forefront of coordinating the response to this outbreak, supported by the NCDC and other partnering agencies.
Preparedness for an outbreak should commence ahead of an outbreak season. Firstly, risk mapping should be carried out to provide insight on the vulnerability of the state/populace for an outbreak or a specific outbreak. Preparedness activities for cholera should cut across all thematic areas as this will give a holistic approach in identifying resources required for preparedness. This includes:
1. Coordination: Developing a preparedness plan to guide activities and understand expectations/roles of every tier of government; Involvement of all identified key stakeholders; Early sensitization and planning with a Rapid Response Team (RRT); Forecasting, planning and coordination with stakeholders on interim measures to be put in place in the eventuality of a large outbreak e.g. setting up of interim water supply, rapid requisition and distribution of commodities for unexpected upsurge of cases, maintaining good hygiene conditions(personal and environmental).
2. Surveillance: Increased alert for Cholera by sensitizing the surveillance teams at the Local and State Government levels. This can be done through Capacity building; Adequate supply and distribution of data collection tools to all health facilities; Improve effective communication channels for receiving reports/information and feedback; Development of a data management system for better and quicker data analysis; Improvement of bio-surveillance activities for rumour capturing and verifications; Consolidating measures for active case search.
3. Case Management: Review of existing guidelines and protocols; Identification/designation of Cholera treatment centres and a case management team at the local and state government levels; Capacity building on case management and Infection, Prevention and Control team.
4.Laboratory: Identification of secondary, tertiary and public health laboratories with testing capacities, (stool testing and water analysis); Request and distribution of test-kits to Cholera endemic/Cholera prone areas for immediate response; Request and distribution of transport medium for specimen; Capacity building of identified laboratory staff in sample collection and transportation.
5. Logistics: Early forecast of outbreak commodities required; Mapping and pre-positioning of commodities e.g. intravenous fluids, in states based on data review of previous outbreaks; Stockpiling and distribution of antibiotics based on review previous epidemiological reports for previous outbreaks
6. Risk Communications: Development of a risk communication plan; Pre-outbreak sensitization and mobilization; Design of communication tools specific for target audience; Early engagement of the mass media for sensitization program and improved/extended use of communication tools
It is important to note that preparedness for any disease outbreak or event of public health concern is an intensive process which requires a multi-sectorial approach, if desired health outcomes are to be achieved. The NCDC held a Cholera preparedness workshop covering the thematic areas listed above, with State Epidemiologists from the eight most affected States, academia and partners. The Cholera preparedness plan and guidelines is being finalised and will guide actions during this outbreak. A Cholera alert letter has also been sent to all State Commissioners of Health and Epidemiologists, alerting them of the season and actions to take. We will continue to provide support, collaborate and guidance to states in preparedness and response activities for an outbreak. States are expected to coordinate these activities to ensure meaningful and sustainable results are achieved.
In the reporting week:
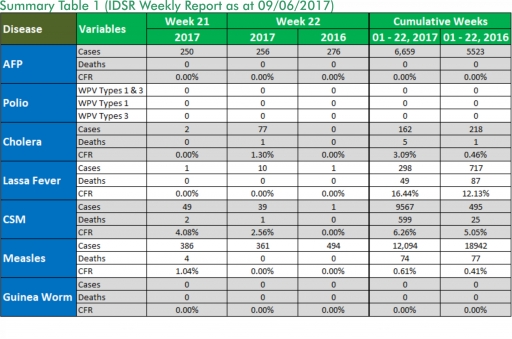
o There were 256 new cases of Acute Flaccid Paralysis (AFP) reported. None was confirmed as Polio. The last reported case of Polio in Nigeria was in August 2016. Active case search for AFP is being intensified as Nigeria has assiduously reinvigorated its efforts at eradicating Polio.
o 77 suspected cases of Cholera were reported from four LGAs in two States and one death was recorded.
o There were 42 suspected cases of Cerebrospinal Meningitis (CSM) reported from 22 LGAs in ten States. Of these, one was laboratory confirmed and one deaths was recorded. Ongoing surveillance for CSM has been intensified in the States.
o There were 361 suspected cases of Measles reported from 33 States. None was laboratory confirmed and four deaths were recorded.
In the reporting week, Enugu and Jigawa States failed to report. Timeliness of reporting increased from 81% in the previous week to 82% while completeness increased from 99% in the previous week to 100%. It is very important for all States to ensure timely and complete reporting at all times, especially during an outbreak.
1. Lassa fever
Please note that the data reflects the routine reports i.e. all suspected cases including the laboratory positive and negative cases
1.1. Ten suspected cases of Lassa fever with four Lab confirmed were reported from eight LGAs (five States) in week 22, 2017 compared with one suspected case from Karu LGA (Nasarawa State) at the same period in 2016.
1.2. Laboratory results of the ten suspected cases were four positives (Edo – 4) and six negatives (Katsina – 3, Kogi – 1, Ogun – 1 & Taraba – 1).
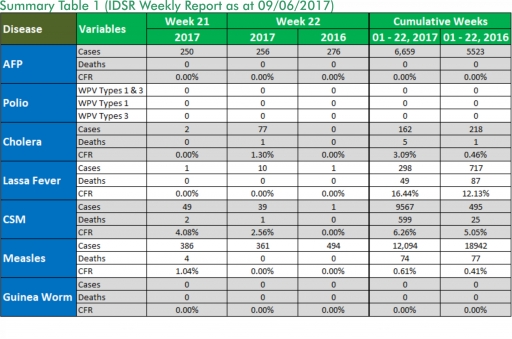
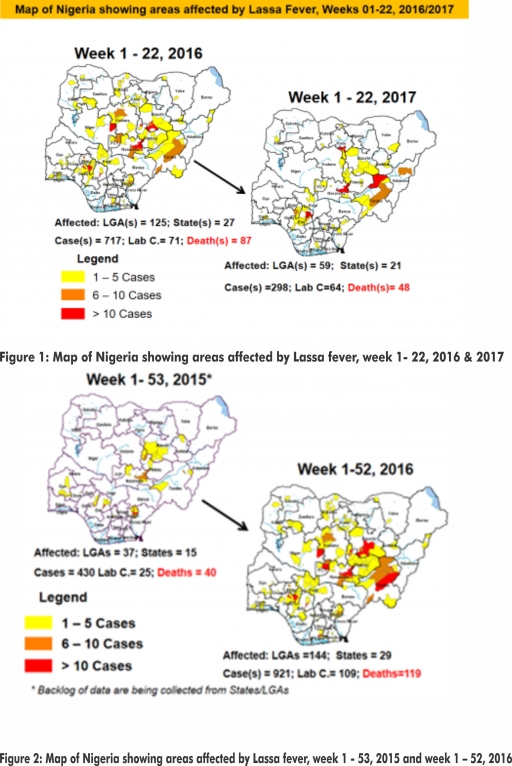
1.3. Between weeks 1 and 22 (2017), 298 suspected Lassa fever cases with 64 laboratory confirmed cases and 49 deaths (CFR, 16.44%) from 59 LGAs (21 States) were reported compared with 717 suspected cases with 71 laboratory confirmed cases and 87 deaths (CFR, 12.15%) from 125 LGAs (27 States) during the same period in 2016 (Figure 1).
1.4. Between weeks 1 and 52 2016, 921 suspected Lassa fever cases with 109 laboratory confirmed cases and 119 deaths (CFR, 12.92%) from 144 LGAs (28 States and FCT) were reported compared with 430 suspected cases with 25 laboratory confirmed cases and 40 deaths (CFR, 9.30%) from 37 LGAs (14 States and FCT) during the same period in 2015 (Figure 2).
1.5. Investigation and active case search ongoing in affected States with coordination of response activities by the NCDC with support from partners.
1.5.1. National Lassa Fever Working Group meeting and weekly National Surveillance and Outbreak Response meeting on-going at NCDC to keep abreast of the current Lassa fever situation in the country.
1.5.2. Response materials for VHFs prepositioned across the country by NCDC at the beginning of the dry season
1.5.3. New VHF guidelines have been developed by the NCDC (Interim National Viral Haemorrhagic Fevers Preparedness guidelines and Standard Operating Procedures for Lassa fever management)
1.5.4. Ongoing reclassification of reported Lassa fever cases
1.5.5. Ongoing review of the variables for case-based surveillance for VHF
1.5.6. VHF case-based forms completed by affected States are being entered into the new VHF management system. This system allows for the creation of a VHF database for the country.
1.5.7. NCDC team sent to Edo State to support Lassa fever data harmonization & Updating of VHF case-based management database
1.5.8. Confirmed cases are being treated at identified treatment/isolation centres across the States with Ribavirin and necessary supportive management also instituted
1.5.9. Onsite support was earlier provided to Ogun, Nasarawa, Taraba, Ondo and Borno States by the NCDC and partners
1.5.10. Offsite support provided by NCDC/partners in all affected States
1.5.11. States are enjoined to intensify surveillance
2. MEASLES
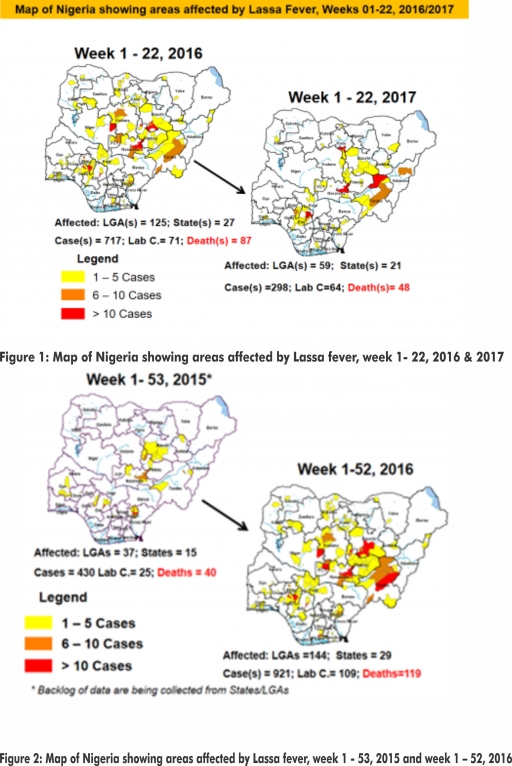
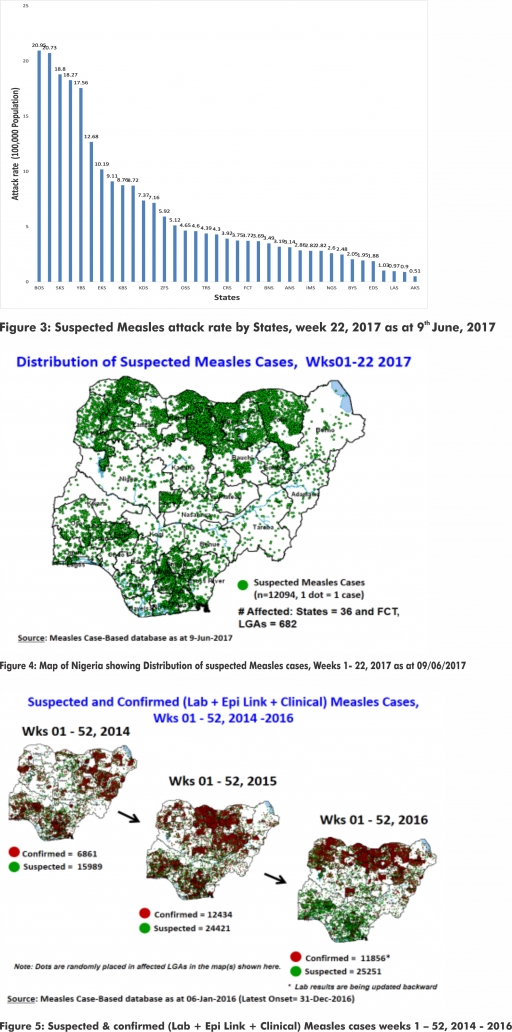
2.1. In the reporting week, 361 suspected cases of Measles were reported from 33 States compared with 494 suspected measles cases from 30 States during the same period in 2016.
2.2. So far, 12,094 suspected Measles cases with 71 laboratory confirmed cases and 74 deaths (CFR, 0. 61%) have been reported in 2017 from 36 States and FCT (Figure 4) compared with 18,942 suspected cases and 77 deaths (CFR, 0.41%) from 36 States and FCT during the same period in 2016.
2.3. In 2016 (week 1 -52), 25,251 suspected Measles cases with 102 deaths (CFR, 0.40%) were reported from 36 States and FCT compared with 24,421 suspected cases with 127 deaths (CFR, 0.52%) during the same period in 2015 (Figure 5)
2.4. Response measures include immunization for all vaccine-preventable diseases in some selected/affected wards/LGAs during SIAs, as well as case management.
2.5. Scheduled Measles campaigns in the North East were conducted from 12th – 17th January, 2017 in Adamawa, Borno and Yobe States (Phase I) and Phase II from 21st – 25th January, 2017 in Borno State and 4th – 8th February, 2017 in Yobe State
3. POLIOMYELITIS
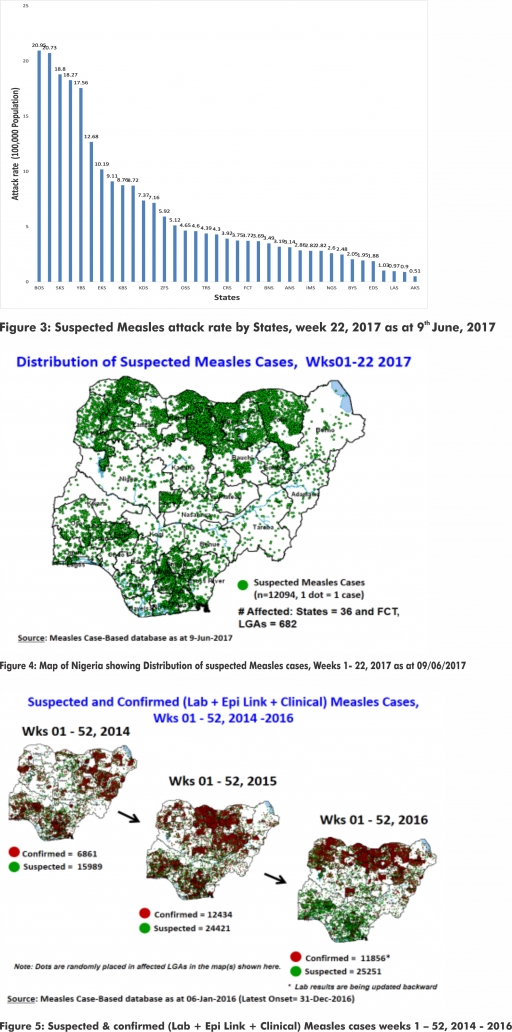
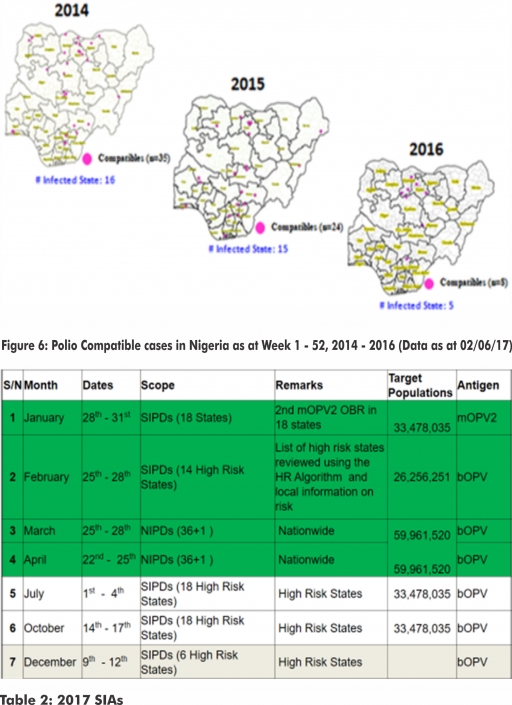
3.1. As at June 2nd 2017, no new case of WPV was recorded
3.2. Three new cVDPV2, environmental derived and Polio compatible cases identified
3.2.1. In the reporting week, 256 cases of AFP were reported from 196 LGAs in 34 States and FCT
3.2.2. AFP Surveillance has been enhanced and outbreak response is on-going in Borno and other high risk States
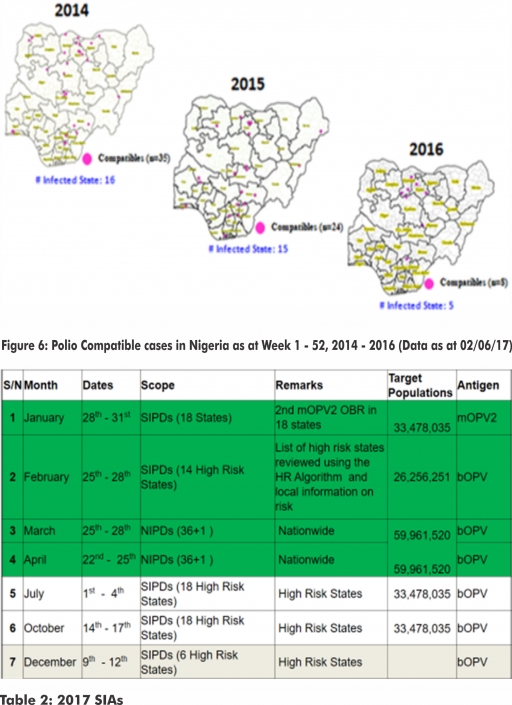
3.2.3. The 1st round of SIPDs in 2017 was conducted from 28th – 31st January 2017 in the 18 high risk States. This was carried out using mOPV2 (2nd mOPV2 OBR). The schedule for other SIAs is as described in Table 2
3.2.4. The 2nd round of SIPDs completed (25th-28th February, 2017) in 14 high risk States using bOPV.
3.2.5. The 1st and 2nd rounds of NIPDs completed (from 25th – 28th March, 2017 and 22nd – 25th April, 2017) nationwide respectively.
3.2.6. Between weeks 1 and 52 in 2016, four WPVs were isolated from Borno State compared to no WPV isolated during the same period in 2015.
3.3. No circulating Vaccine Derived Polio Virus type 2 (cVDPV2) was isolated in week 1 - 52, in both 2016 and 2015.
3.4. Between weeks 1 and 52, 2016 two (2) cVDPV2 were isolated in two LGAs (two States) while one (1) cVDPV2 was isolated from Kwali, FCT during the same period in 2015.
3.5. Six confirmed WPVs were isolated in 2014.
3.6. The SIAs were strengthened with the following events:
3.6.1. Immunization for all vaccine-preventable diseases in some selected wards/LGAs.
3.6.2. Use of health camp facilities.
3.6.3. Field supportive supervision and monitoring.
3.6.4. Improved Enhanced Independent Monitoring (EIM) and Lots Quality Assessments (LQAs) in all Polio high risk States.
3.6.5. High level of accountability framework
4. CHOLERA
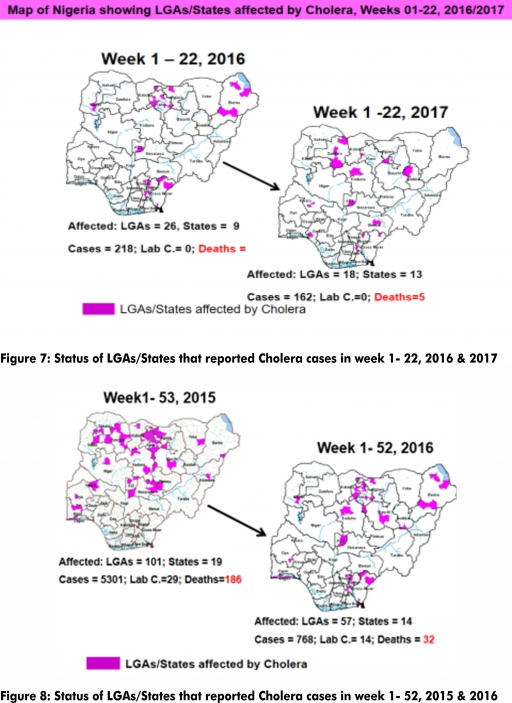
4.1. 77 suspected cases of Cholera and one death were reported from four LGAs (two State) in week 22 compared with zero case at the same period in 2016.
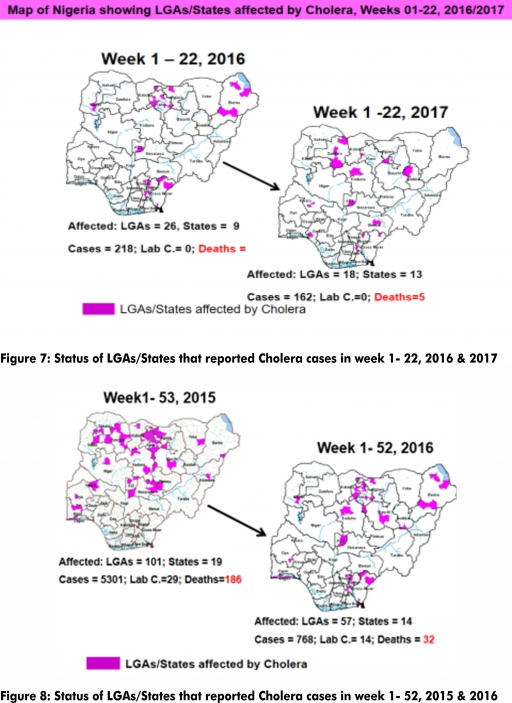
4.2. Between weeks 1 and 22 (2017), 162 suspected Cholera cases and five deaths (CFR, 3.09%) from 18 LGAs (13 States) were reported compared with 218 suspected cases and one death (CFR, 0.46%) from 26 LGAs (nine States) during the same period in 2016 (Figure 7).
4.3. Between weeks 1 and 52 (2016), 768 suspected Cholera cases with 14 laboratory confirmed cases and 32 deaths (CFR, 4.17%) from 57 LGAs (14 States) were reported compared with 5,301 cases with 29 laboratory confirmed cases and 186 deaths (CFR, 3.51%) from 101 LGAs (18 States and FCT) during the same period in 2015 (Figure 8).
4.4. Cholera preparedness workshop held from 31st May – 1st June, 2017 in Abuja to
develop Cholera preparedness plan as the season set in.
4.5. NCDC/partner are providing onsite support to Kwara State.
4.6. States are enjoined to intensify surveillance.
5. CEREBROSPINAL MENINGITIS (CSM)
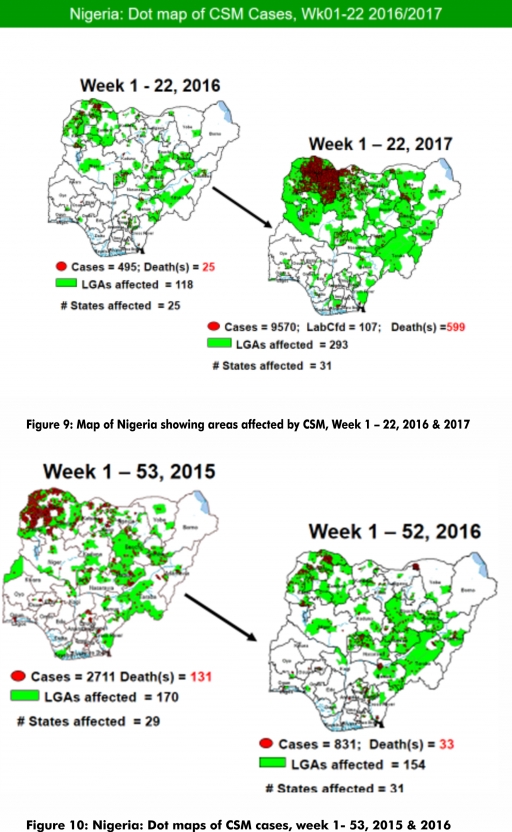
5.1. In the reporting week 22, 42 suspected Cerebrospinal Meningitis (CSM) cases with one laboratory confirmed case and one deaths (CFR, 2.56%) were reported from 22 LGAs (10 States) compared with one suspected case from Bukuru LGA (Benue States) at the same period in 2016.
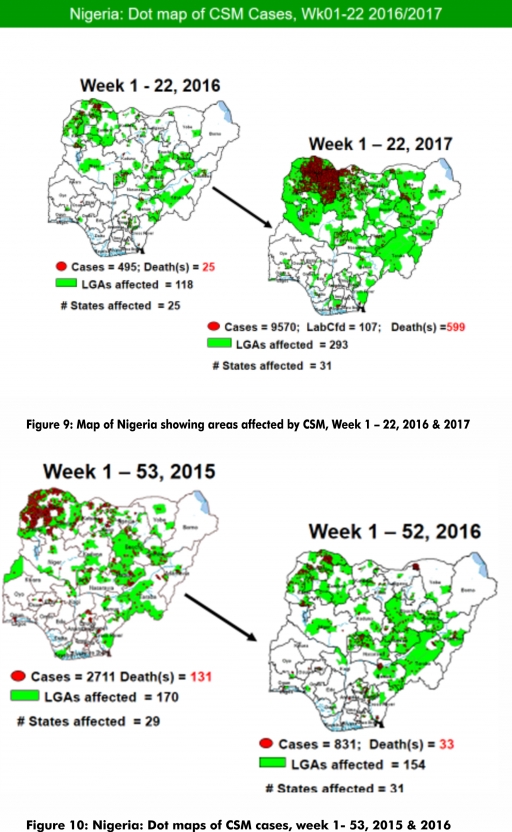
5.2. Between weeks 1 and 22 (2017), 9570 suspected CSM cases with 107 laboratory confirmed cases and 599 deaths (CFR, 6.26%) were recorded from 293 LGAs (31 States) compared with 495 suspected cases and 25 deaths (CFR, 5.05%) from 118 LGAs (25 States) during the same period in 2016 (Figure 9).
5.3. Between weeks 1 and 52, 2016, 831 suspected CSM cases with 43 laboratory confirmed cases and 33 deaths (CFR, 3.97%) were recorded from 154 LGAs (30 States and FCT) compared with 2,711 suspected cases and 131 deaths (CFR, 4.83%) from 170 LGAs (28 States and FCT) during the same period in 2015 (Figure 10)
5.4. Timeliness/completeness of CSM case-reporting from States to the National Level (2017 versus 2016): on average, 79.4% of the 26 endemic States sent CSM reports in a timely manner while 97.9% were complete in week 1 – 22, 2017 as against 82.5% timeliness and 98.4% completeness recorded within the same period in 2016
5.5. CSM preparedness checklist sent to 36 States and FCT ahead of 2017 meningitis season
5.6. Confirmed cases are being treated at identified treatment centres in affected States (Zamfara, Sokoto, Katsina, Kebbi, Niger, Kano, Yobe and Jigawa) and necessary supportive management also instituted
5.7. CSM National Emergency Operations Centre constituted at the Nigeria Centre for Disease Control
5.8. Onsite support was earlier provided to Zamfara, Sokoto, Katsina, Kebbi, Kano, Yobe and Niger States by NCDC and partners
5.9. Ongoing offsite support to States
5.10. Intensive Surveillance is on-going in high risk States.
5.11. Reactive vaccination completed in Zamfara State for people aged one to 29 years using polysaccharide meningococcal A & C vaccine.
5.12. Reactive vaccination completed in two wards (Gada and Kaffe) in Gada LGA in Sokoto State using polysaccharide meningococcal A & C vaccine for people aged two to 29 years.
5.13. Reactive vaccination completed in nine LGAs in Sokoto State using monosaccharide meningococcal conjugate C vaccine for aged one to 20 years.
5.14. Reactive vaccination campaign completed in Yobe State and the second phase of the campaign in Zamfara State also completed.
5.15. Training and deployment of first batch of medical teams to support case management in Sokoto and Zamfara States completed (from Friday 5th - 26th May, 2017).
5.16. Deployed mobile testing laboratory to Zamfara State to aid diagnosis
5.17. Team deployed by NCDC/WHO to support surveillance activities, laboratory data harmonization and monitoring of the implementation plan in Yobe state completed their assessment.
6. GUINEA WORM DISEASE
6.1. In the reporting week, no rumour report of Guinea Worm disease was received from any State.
6.2. Nigeria has celebrated eight consecutive years of zero reporting of Guinea worm disease in the country. The Country has been officially certified free of Dracunculiasis transmission by the International Commission for the Certification of Dracunculiasis Eradication (ICCDE).
(For further information, contact NIGEP NC/Director: Mrs. I, Anagbogu: +2348034085607, [email protected])
FOR MORE INFORMATION CONTACT
Surveillance Unit:
Nigeria Centre for Disease Control
801 Ebitu Ukiwe Street, Jabi, Abuja, Nigeria.
[email protected]
www.ncdc.gov.ng/reports
0800-970000-10




 Toll Free Number: 6232
Toll Free Number: 6232 Whatsapp: +234 708 711 0839
Whatsapp: +234 708 711 0839 SMS Number: +234 809 955 5577
SMS Number: +234 809 955 5577 