The response to outbreaks usually involves multiple activities, many of which occur concurrently. In most situations, resources are scarce and few personnel are involved or available to respond to an outbreak. For effective outbreak management, a well-defined structure needs to be established.
An Emergency Operations Centre (EOC) is a structure set up for the preparation, coordination, and management of response activities for public health events. It is also known as an incident command centre (ICC) and can operate in three different modes-Watch, Alert and Response Modes. These different modes function based on information received by the EOC on public health events. An Incident Manager (IM) is usually appointed as the lead in an EOC and is responsible for proper allocation of resources, aligning of activities, facilitating EOC meetings and production/approval of outbreak-related documentation
1. Watch Mode: The Watch mode staff are available and are involved in event based surveillance and documentation of events as they occur. Based on information received, certain actions/tasks are escalated to appropriate EOC personnel. At this point, Sitreps and Spotreps are generated and shared with relevant key stakeholders.
2. Alert Mode: At this point, subject matter experts (SMEs) are contacted. Surveillance is enhanced and notifications generated. A preliminary assessment team is convened and coordination with other ministries is initiated. An incident action plan is developed with deployment preparations initiated. In an alert phase, a rapid response team may be deployed for initial assessment.
3. Response Mode: The EOC is activated and the incident manager is appointed. The incident management staff and SMEs are mobilized. All liaisons with other relevant ministries are established. Resources are deployed and the incident action plan is finalized with specific timelines for stated activities. A situational awareness is conducted and reports generated are usually response-specific.
It is important to note that an EOC can exist in the three different modes for different incidents/events. This helps with optimal utilization of resources and proper alignment of activities.
The Nigeria Centre for Disease Control (NCDC) has recently set up its Incident Coordination Centre (ICC), which has improved the surveillance and response to public health threats and incidents. The replication of this at the State level will greatly contribute to a stronger and better-coordinated response to outbreaks in the country.
Recently, the NCDC supported the Katsina State Government in establishing a state-owned EOC to be used for coordination of all outbreaks/public events in the state, starting with Cerebrospinal Meningitis (CSM).
It is important for all States in the country, to adapt the EOC structure to ensure better coordination, and contribute to national health security.
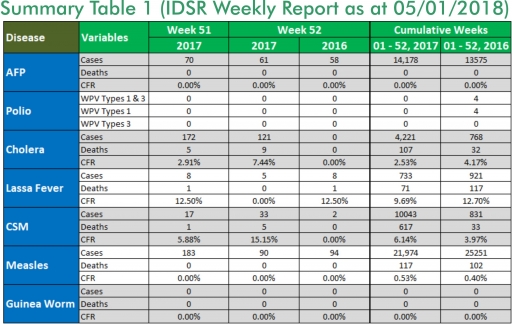
In the reporting week ending on December 31, 2017:
o There were 61 new cases of Acute Flaccid Paralysis (AFP) reported. None was confirmed as Polio. The last reported case of Polio in Nigeria was in August 2016. Active case search for AFP is being intensified as Nigeria has reinvigorated its efforts at eradicating Polio.
o 121 suspected cases of Cholera were reported from 18 LGAs in Kano State. Of these, five were laboratory confirmed and nine deaths were recorded.
o Five suspected cases of Lassa fever were reported from four LGAs in three States (Bauchi – 2, Edo – 1 & Kogi – 2). One was laboratory confirmed and no death was recorded.
o There were 33-suspected cases of Cerebrospinal Meningitis (CSM) reported from 18 LGAs in four States (Kaduna – 2, Katsina - 7, Sokoto – 2 & Zamfara – 22). Of these, nine were laboratory confirmed and five deaths were recorded. Ongoing surveillance for CSM has been intensified in all the 26 States in the Nigeria meningitis belt and case-based surveillance commenced from 4th December 2017.
o There were 90- suspected cases of Measles reported from 21 States. None was laboratory confirmed and no death was recorded.
In the reporting week, all States sent in their report. This is a remarkable improvement! Timeliness of reporting remains 86% in both previous and current weeks (Week 51 and 52) while completeness remains at 100%. It is very important for all States to ensure timely and complete reporting at all times, especially during an outbreak.
1. LASSA FEVER
Please note that the data reflects the routine reports i.e. all suspected cases including the laboratory positive and negative cases
1.1. Five suspected cases of Lassa fever with one Laboratory confirmed were reported from four LGAs (three States: Bauchi – 2, Edo – 1 & Kogi – 2) in week 52, 2017 compared with eight suspected cases and one death (CFR, 12.50%) reported from six LGAs (five States) at the same period in 2016
1.2. Laboratory results of the five suspected cases; one positive for Lassa fever (Edo – 1), four were negative for Lassa fever & other VHFs (Bauchi – 2 & Kogi – 2)
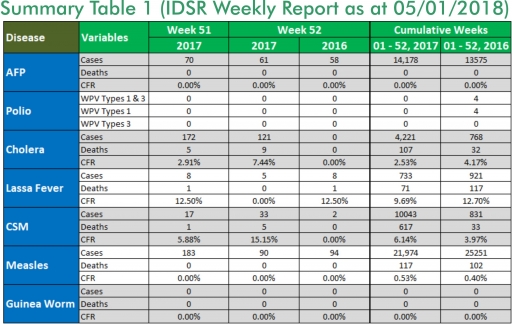
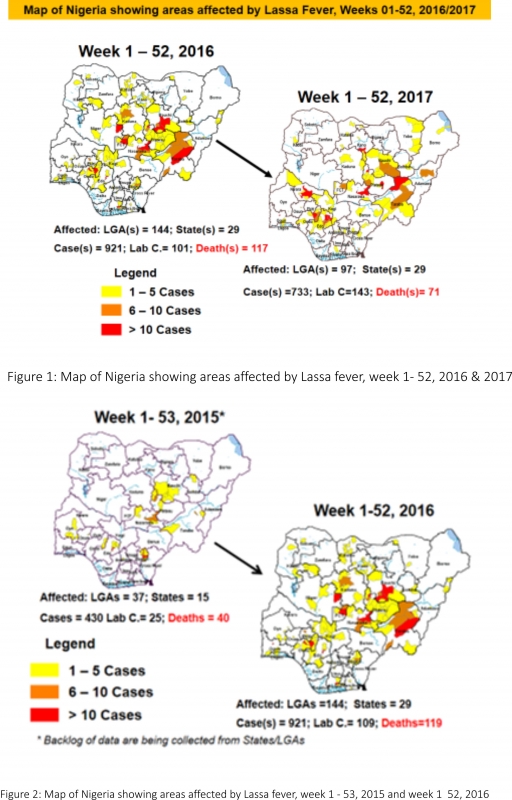
1.3. Between weeks 1 and 52 (2017), 733 suspected Lassa fever cases with 143 laboratory confirmed cases and 71 deaths (CFR, 9.69%) from 97 LGAs (29 States) were reported compared with 921 suspected cases with 101 laboratory confirmed cases and 117 deaths (CFR, 12.70%) from 144 LGAs (29 States) during the same period in 2016 (Figure 1)
1.4. Between weeks 1 and 52 2016, 921 suspected Lassa fever cases with 109 laboratory confirmed cases and 119 deaths (CFR, 12.92%) from 144 LGAs (28 States and FCT) were reported compared with 430 suspected cases with 25 laboratory confirmed cases and 40 deaths (CFR, 9.30%) from 37 LGAs (14 States and FCT) during the same period in 2015 (Figure 2)
1.5. Investigation and active case search ongoing in affected States with coordination of response activities by the NCDC with support from partners
1.5.1. National Lassa Fever Working Group meeting and weekly National Surveillance and Outbreak Response meeting on-going at NCDC to keep abreast of the current Lassa fever situation in the country
1.5.2. Response materials for VHF provided to support States
1.5.3. National VHF guidelines (National Viral Haemorrhagic Fevers Preparedness guidelines, Infection Prevention and Control of VHF and Standard Operating Procedures for Lassa fever management) are available on the NCDC website- http://ncdc.gov.ng/diseases/guidelines
1.5.4. VHF case-based forms completed by affected States are being entered into the new VHF management system. This system allows for the creation of a VHF database for the country. Data from the VHF database is currently being analysed to inform decision making in the coming year
1.5.5. States are enjoined to intensify surveillance and promote Infection, Prevention and Control (IPC) measures in health facilities
1.5.6. NCDC Lassa fever working group visited priority States, to provide support in developing preparedness and response plans ahead of dry season
2. MEASLES
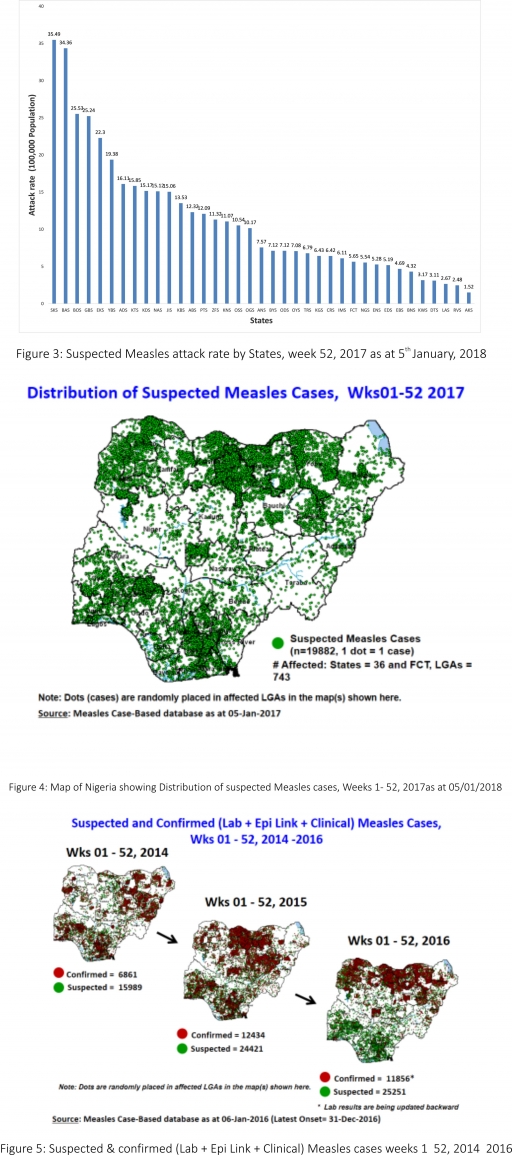
2.1. In the reporting week, 90 suspected cases of Measles were reported from 21 States compared with 94 suspected cases reported from 16 States during the same period in 2016
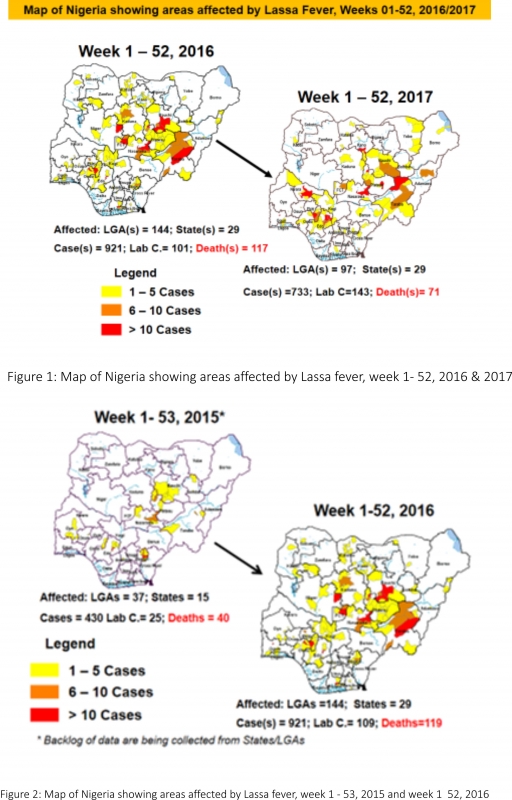
2.2. So far, 21,974 suspected Measles cases with 109 laboratory confirmed cases and 117 deaths (CFR, 0. 53%) have been reported in 2017 from 36 States and FCT (Figure 4) compared with 25,251 suspected cases and 102 deaths (CFR, 0.40%) from 36 States and FCT during the same period in 2016
2.3. In 2016 (week 1 -52), 25,251 suspected Measles cases with 102 deaths (CFR, 0.40%) were reported from 36 States and FCT compared with 24,421 suspected cases with 127 deaths (CFR, 0.52%) during the same period in 2015 (Figure 5)
2.4. Response measures include immunisation for all vaccine-preventable diseases in some selected/affected wards/LGAs during SIAs, as well as case management
2.5. Scheduled Measles campaigns in the North East were conducted from 12th – 17th January 2017 in Adamawa, Borno and Yobe States (Phase I) and Phase II from 21st – 25th January 2017 in Borno State and 4th – 8th February 2017 in Yobe State
2.6. Measles mass campaign conducted in seven North West and North East States from 9th – 14th November 2017 and 30th November – 5th December 2017 respectively.
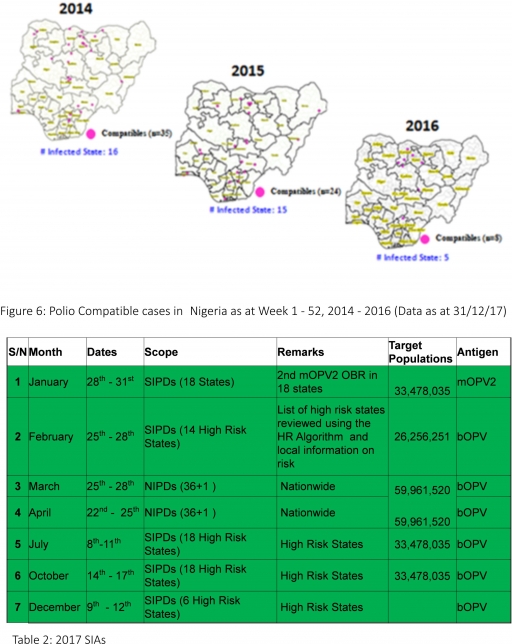
3. POLIOMYELITIS
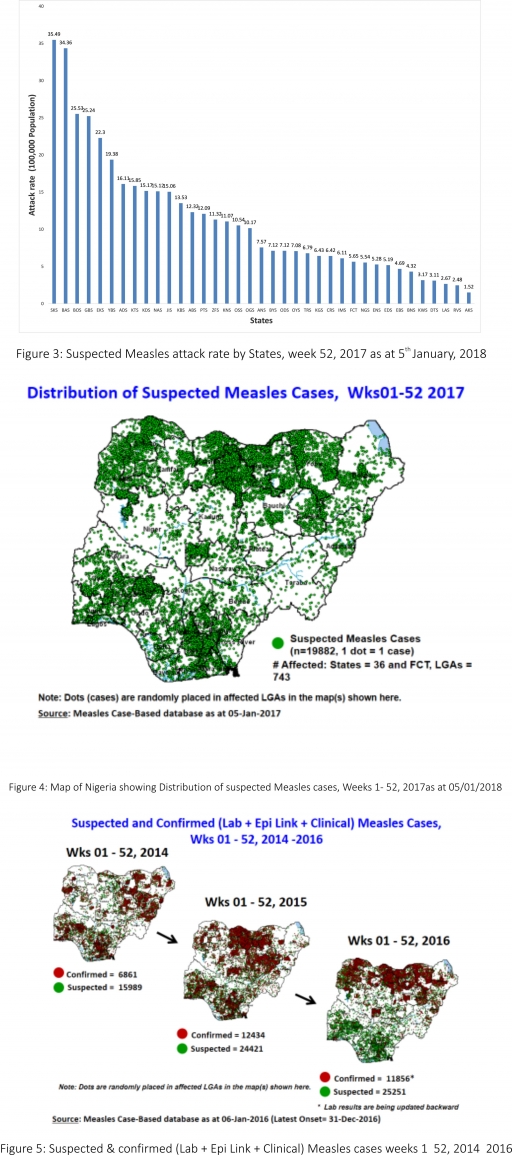
3.1. As at December 31st, 2017, no new case of WPV was recorded
3.2. Three new cVDPV2, environmental derived and Polio compatible cases identified
3.2.1. In the reporting week, 61 cases of AFP were reported from 57 LGAs in 21 States and FCT
3.2.2. AFP Surveillance has been enhanced and outbreak response is on-going in Borno and other high-risk States
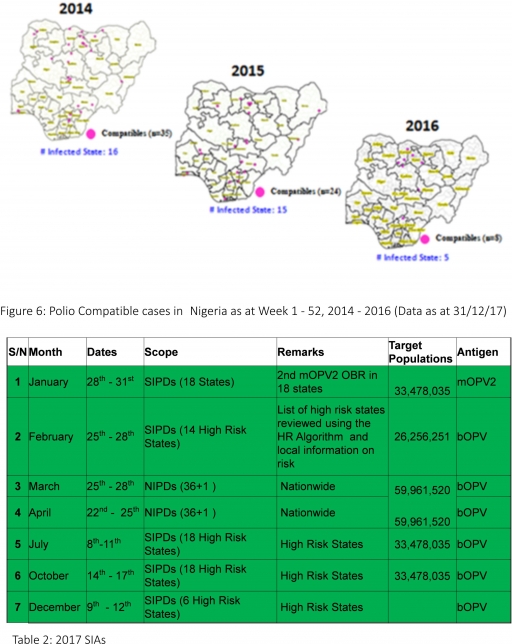
3.2.3. The 1st round of SIPDs in 2017 was conducted from 28th – 31st January 2017 in the 18 high-risk States. This was carried out using mOPV2 (2nd mOPV2 OBR). The schedule for other SIAs is as described in Table 2
3.2.4. The 2nd and 3rd round of SIPDs completed (25th-28th February and 8th – 11th July 2017) in 14 & 18 high-risk States using bOPV respectively.
3.2.5. The 1st and 2nd rounds of NIPDs completed (from 25th – 28th March 2017 and 22nd – 25th April 2017) nationwide respectively.
3.2.6. The 4th round of SIPDs completed from 14th- 17th October 2017 in 18 high-risk States using bOPV.
3.2.7. The 5th round of SIPDs completed from 9th- 12th December 2017 in 6 high-risk States using bOPV.
3.2.8. Between weeks 1 and 52 in 2016, four WPVs were isolated from Borno State compared to no WPV isolated during the same period in 2015.
3.3. No circulating Vaccine Derived Polio Virus type 2 (cVDPV2) was isolated in week 1 - 52, in both 2016 and 2015.
3.4. Between weeks 1 and 52, 2016 two (2) cVDPV2 were isolated in two LGAs (two States) while one (1) cVDPV2 was isolated from Kwali, FCT during the same period in 2015.
3.5. Six confirmed WPVs were isolated in 2014.
3.6. The SIAs were strengthened with the following events:
3.6.1. Immunisation for all vaccine-preventable diseases in some selected wards/LGAs.
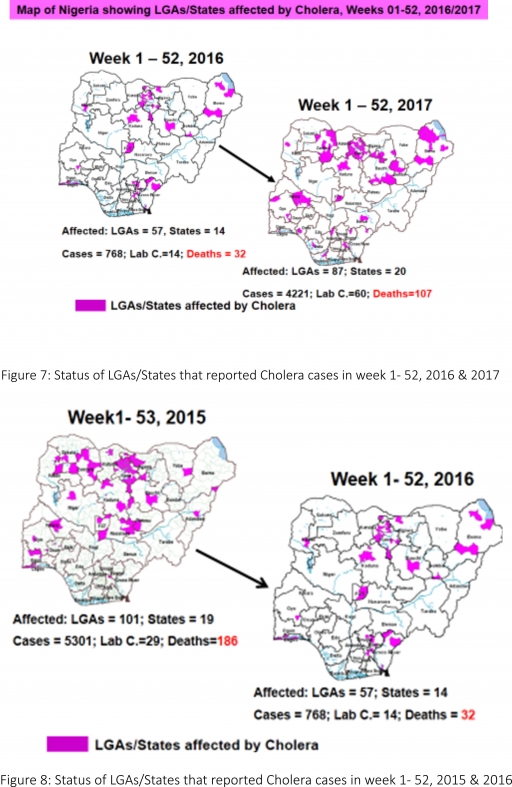
4. CHOLERA
4.1. 121 suspected cases of Cholera with five Laboratory confirmed and nine deaths (CFR, 7.44%) were reported from 18 LGAs (Kano State) in week 52 compared with zero cases reported during the same period in 2016.
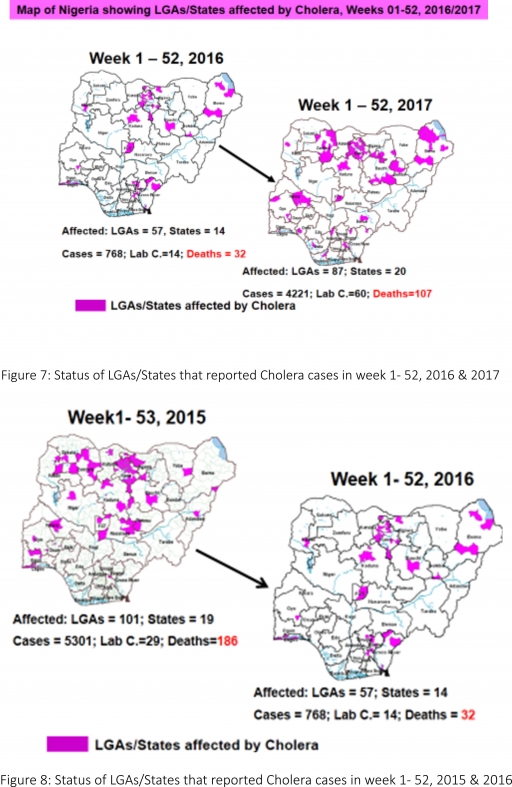
4.2. Between weeks 1 and 52 (2017), 4221 suspected Cholera cases with 60 laboratory confirmed and 107 deaths (CFR, 2.53%) from 87 LGAs (20 States) were reported compared with 768 suspected cases and 32 deaths (CFR, 4.17%) from 57 LGAs (14 States) during the same period in 2016 (Figure 7).
4.3. Between weeks 1 and 52 (2016), 768 suspected Cholera cases with 14 laboratory confirmed cases and 32 deaths (CFR, 4.17%) from 57 LGAs (14 States) were reported compared with 5,301 cases with 29 laboratory confirmed cases and 186 deaths (CFR, 3.51%) from 101 LGAs (18 States and FCT) during the same period in 2015 (Figure 8).
4.4. National Preparedness and Response to Acute Watery Diarrhoea/ Cholera Guidelines have been finalised: http://ncdc.gov.ng/themes/common/docs/protocols/45_1507196550.pdf
4.7. States are enjoined to intensify surveillance, implement WASH activities and ensure early reporting.
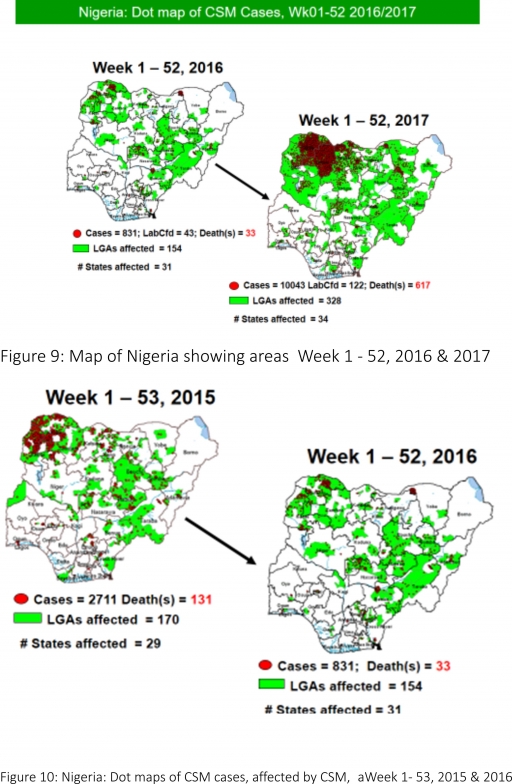
5. CEREBROSPINAL MENINGITIS (CSM)
5.1 In the reporting week 52, 33 suspected Cerebrospinal Meningitis (CSM) cases with nine Laboratory confirmed and five death (CFR, 15.15%) were reported from 18 LGAs (four States; Kaduna – 2, Katsina - 7, Sokoto – 2 & Zamfara - 22) compared with two suspected cases from Nguru LGA (Yobe State) at the same period in 2016
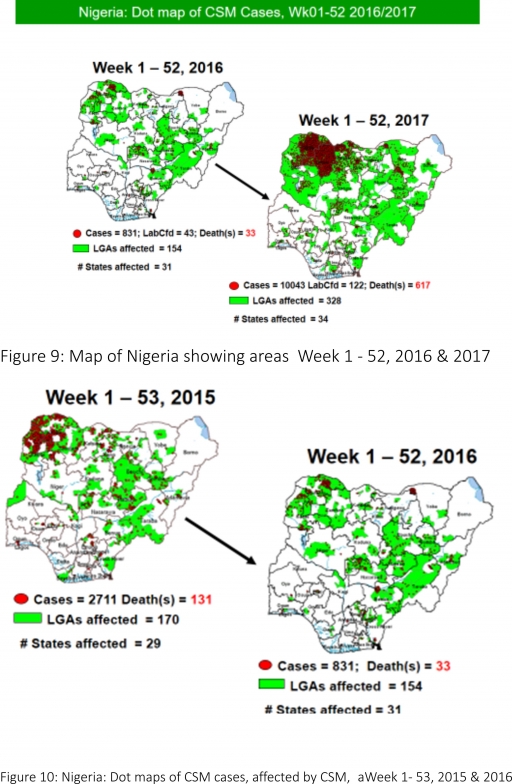
5.2 Between weeks 1 and 52 (2017), 10043 suspected CSM cases with 122 laboratory confirmed cases and 617 deaths (CFR, 6.14%) were recorded from 328 LGAs (34 States) compared with 831 suspected cases and 33 deaths (CFR, 3.97%) from 154 LGAs (31 States) during the same period in 2016 (Figure 9)
5.3 Between weeks 1 and 52, 2016, 831 suspected CSM cases with 43 laboratory confirmed cases and 33 deaths (CFR, 3.97%) were recorded from 154 LGAs (30 States and FCT) compared with 2,711 suspected cases and 131 deaths (CFR, 4.83%) from 170 LGAs (28 States and FCT) during the same period in 2015 (Figure 10)
5.4 Timeliness/completeness of CSM case-reporting from States to the National Level (2017 versus 2016): on average, 83.4% of the 26 endemic States sent CSM reports in a timely manner while 98.7% were complete in week 1 – 52, 2017 as against 84.8% timeliness and 97.9% completeness recorded within the same period in 2016
5.5 The National CSM Emergency Operations Centre has been activated and is currently in response mode
5.6 Enhanced surveillance/ case based surveillance began 1st of December 2017
5.7 Rapid Response Teams currently deployed to support response in Zamfara and Katsina States
5.8 The National CSM Guidelines have been finalised and available via http://ncdc.gov.ng/themes/common/docs/protocols/51_1510449270.pdf
5.9 Development of State-specific CSM Epidemic Preparedness & Response plan completed in 11 Northern States within the Meningitis belt
6 GUINEA WORM DISEASE
6.1 In the reporting week, no rumour report of Guinea Worm disease was received from any State.
6.2 Nigeria has celebrated eight consecutive years of zero reporting of Guinea worm disease in the country. The Country has been officially certified free of Dracunculiasis transmission by the International Commission for the Certification of Dracunculiasis Eradication (ICCDE).
(For further information, contact Nigeria Guinea Worm Eradication Program / Neglected Tropical Diseases Division, Public Health Department/Federal Ministry of Health)
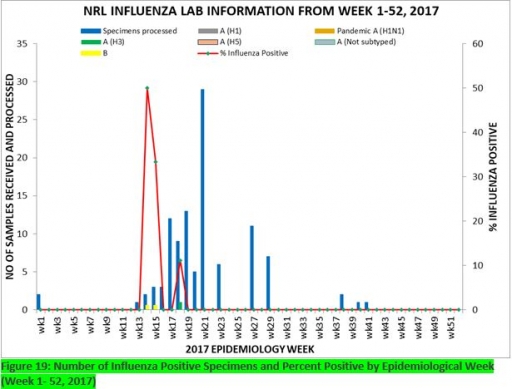
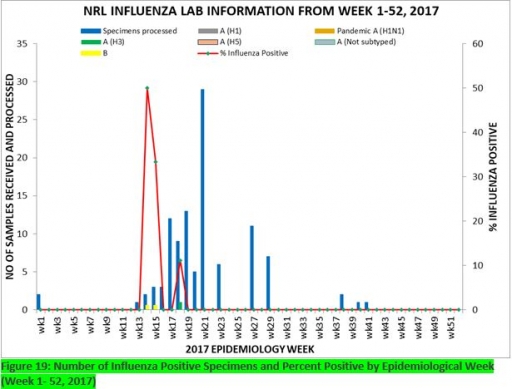
7. Update on national Influenza sentinel surveillance, Nigeria week 1 - 52, 2017
7.1. From week 1-52, 150-suspected cases were reported, of which 148 were Influenza-like-illness (ILI), eight Severe Acute Respiratory Infection (SARI).
7.2 150 samples were received of which 107 were processed. Of the processed samples, 99(92.5%) were ILI cases, eight (7.5%) were Severe Acute Respiratory Infection (SARI).
7.4. Of the 99 processed ILI samples, 1(1.01%) was positive for Influenza A; two (2.02%) positive for Influenza B and 96(96.97%) were negative.
7.5. Of the eight processed SARI samples, none was positive for Influenza A and Influenza B.
7.6. Three (2.80%) of the processed 107 samples were positive for Influenza, with one (33.3%) of these positive for Influenza A and two (66.7%) positive for Influenza B.
7.7. The subtypes A seasonal H3, 2009A/H1N1 and A/not subtyped account for (100%), 0 (0.0%) and 0 (0.0%) of the total influenza A positive samples respectively.
7.8. The percentage influenza positive was highest (50.0%) in week 14, 2017
7.9. In the reporting week 50, none samples were left unprocessed
FOR MORE INFORMATION CONTACT
Surveillance Unit:
Nigeria Centre for Disease Control,
801 Ebitu Ukiwe Street, Jabi, Abuja, Nigeria.
[email protected]
www.ncdc.gov.ng/reports
0800-970000-10

 Toll Free Number: 6232
Toll Free Number: 6232 Whatsapp: +234 708 711 0839
Whatsapp: +234 708 711 0839 SMS Number: +234 809 955 5577
SMS Number: +234 809 955 5577 