In Epi-week 37, active case search for suspected cases of yellow fever disease commenced across various communities in Ifelodun LGA in Kwara State. Cases with symptoms that match the case definition of Yellow Fever which includes fever, vomiting, and yellowness of the eyes were described by some members of communities visited. Following this, a total of 43 suspected cases were identified, for which laboratory specimens were collected and are being tested. So far, 30 results are negative with 1 invalid sample and 12 results pending.
There are four major components to managing an outbreak of yellow fever- community mobilization, case management, vector control and reactive vaccination. Editorials for the next four weeks will focus on each of these components with a view to highlighting practical aspects to be utilized as we respond to the current confirmed case. This week’s focus is on Community mobilization.
Community mobilization activities involve creating public awareness (or increase existing awareness) about the disease, targeting a specific population. For a disease such as yellow fever, attention should be paid to cross-border travelers, migrant workers, host communities, forest workers/dwellers and people in hard-to-reach areas. Areas of interest during community mobilization activities can include identifying signs and symptoms of the disease, mode of transmission and preventive measures against the disease.
1. Transmission-Yellow fever is transmitted mainly through the bite of an infected female mosquito, Aedes aegypti. Other vectors of the virus include tiger mosquito(Aedes albopictus), Aedes africanus and Haemogogus species. These different mosquito species live and breed in different habitats-some breed around houses (domestic), others in the jungle (wild), and some in both habitats (semi-domestic). There are 3 transmission cycles
• Sylvatic (or jungle) yellow fever-Monkeys are the primary reservoir of yellow fever are bitten by wild mosquitoes which pass the virus to other monkeys. Occasionally humans working or traveling in the forest are bitten by infected mosquitoes and develop yellow fever.
• Intermediate yellow fever-Semi-domestic mosquitoes (those that breed both in the wild and around households) infect both monkeys and people. Increased contact between people and infected mosquitoes leads to increased transmission. Here, many separate communities can develop outbreaks at the same time.
• Urban yellow fever- Infected persons introduce the virus into heavily populated areas where there is a large mosquito density and people living there have little or no immunity due to lack of vaccination. This usually results in large epidemics. In this case, infected mosquitoes transmit the virus from person to person.
2. Signs and Symptoms-Incubation period are usually 3 to 6 days and over 80% of infected persons are asymptomatic. 10% will present with non-specific symptoms like fever, muscle pain with prominent back pain, headache, loss of appetite, nausea and/or vomiting. These symptoms disappear after 3 to 4 days. However, a small percentage of cases enter the second phase within 24 hours of recovering from initial symptoms. This very toxic phase is characterized by high-grade fever, jaundice(yellowing of the eyes and skin), dark urine and abdominal pain with vomiting. Bleeding can occur from the nose, mouth, eyes or stomach.
3. Prevention-Prevention messages for yellow fever should be centered on vaccination (which offers life-long immunity), mosquito control and outbreak preparedness (for early detection and control) of any outbreaks that may occur. Yellow fever vaccine is included in Nigeria’s routine immunization schedule. A communal effort is ideal for effective preventive measures to be successfully carried out. All travelers in and out of Nigeria must have a valid yellow fever vaccination card.
The Kwara State Ministry of Health is working with the Nigeria Centre for Disease Control (NCDC), National Primary Healthcare Development Agency (NPHCDA), World Health Organisation (WHO) and other partners to bring the current yellow fever outbreak under control. There are plans for a reactive vaccination campaign to be carried out in affected communities as an effort towards outbreak control.
States are enjoined to sustain community mobilisation programs and aim to reach out to all members of the public, particularly susceptible populations e.g. cross-border travelers, forest workers/dwellers, migrant workers and people in hard-to-reach areas. Early reporting of suspected cases of Yellow fever to the next level is very important.
In the reporting week ending on the 17th of September, 2017:
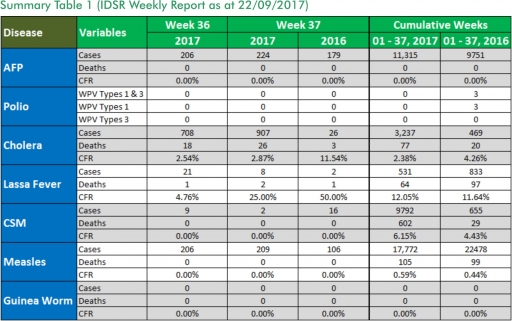
o There were 224 new cases of Acute Flaccid Paralysis (AFP) reported. None was confirmed as Polio. The last reported case of Polio in Nigeria was in August 2016. Active case search for AFP is being intensified as Nigeria has assiduously reinvigorated its efforts at eradicating Polio.
o 907 suspected cases of Cholera were reported from eight LGAs (six States; Bauchi – 2, Borno – 842, Kaduna – 40, Kano – 5, Oyo – 1 and Zamfara - 17). One was laboratory confirmed and 26 deaths were recorded.
o Eight suspected cases of Lassa fever with three Laboratory confirmed and two deaths were reported from five LGAs in four States (Bauchi – 1, Edo – 3, Gombe – 2 andKwara – 2).
o There were two suspected cases of Cerebrospinal Meningitis (CSM) reported from two LGAs in two States (Enugu – 1 and Kogi – 1). Of these, none was laboratory confirmed and no death was recorded. Ongoing surveillance for CSM has been intensified in all the 26 States in the Nigeria meningitis belt.
o There were 209 suspected cases of Measles reported from 29 States. None was laboratory confirmed and no death was recorded.
In the reporting week, Ebonyi and Gombe States failed to send in their report. Timeliness of reporting remains 84% in both previous and current weeks (Week 36 and 37) while completeness remains at 100%. It is very important for all States to ensure timely and complete reporting at all times, especially during an outbreak.
1. Lassa fever
Please note that the data reflects the routine reports i.e. all suspected cases including the laboratory positive and negative cases
1.1. Eight suspected cases of Lassa fever with three Laboratory confirmed and two deaths (CFR, 25.0%) were reported from five LGAs (four States; Bauchi – 1, Edo – 3, Gombe – 2 and Kwara – 2) in week 37, 2017 compared with two suspected cases and one death (CFR, 50.0%) reported from two LGAs (two States) at the same period in 2016.
1.2. Laboratory results of the eight suspected cases were three positives for Lassa fever (Edo -3) while five were negative for Lassa fever and other VHFs (Bauchi – 1, Gombe – 2 and Kwara - 2).
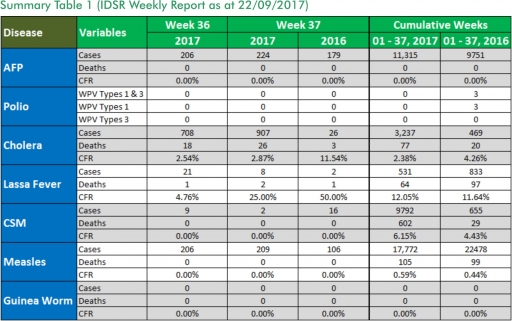
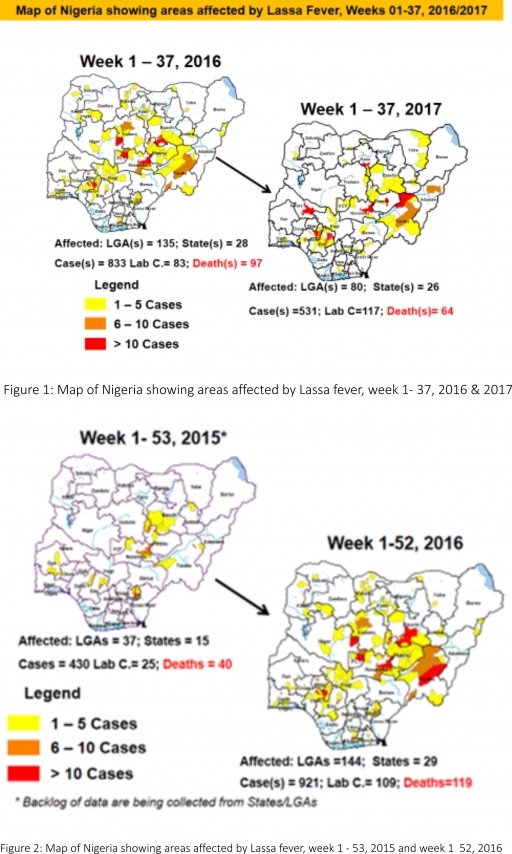
1.3. Between weeks 1 and 37 (2017), 531 suspected Lassa fever cases with 117 laboratory confirmed cases and 64 deaths (CFR, 12.05%) from 80 LGAs (26 States) were reported compared with 833 suspected cases with 83 laboratory confirmed cases and 97 deaths (CFR, 11.64%) from 135 LGAs (28 States) during the same period in 2016 (Figure 1).
1.4. Between weeks 1 and 52 2016, 921 suspected Lassa fever cases with 109 laboratory confirmed cases and 119 deaths (CFR, 12.92%) from 144 LGAs (28 States and FCT) were reported compared with 430 suspected cases with 25 laboratory confirmed cases and 40 deaths (CFR, 9.30%) from 37 LGAs (14 States and FCT) during the same period in 2015 (Figure 2).
1.5. Investigation and active case search ongoing in affected States with coordination of response activities by the NCDC with support from partners.
1.5.1. National Lassa Fever Working Group meeting and weekly National Surveillance and Outbreak Response meeting on-going at NCDC to keep abreast of the current Lassa fever situation in the country.
1.5.2. Response materials for VHFs provided to support States
1.5.3. New VHF guidelines have been developed by the NCDC (National Viral Haemorrhagic Fevers Preparedness guidelines, Infection Prevention and Control of VHF and Standard Operating Procedures for Lassa fever management) and are available on the NCDC website.
1.5.4. National Lassa fever outbreak review meeting carried out with all affected States and partners
1.5.5. Ongoing reclassification of reported Lassa fever cases
1.5.6. Ongoing review of the variables for case-based surveillance for VHF
1.5.7. VHF case-based forms completed by affected States are being entered into the new VHF management system. This system allows for the creation of a VHF database for the country.
1.5.8. Confirmed cases are being treated at identified treatment/isolation centres across the States with Ribavirin and necessary supportive management also instituted
1.5.9. Onsite support was earlier provided to Ogun, Nasarawa, Taraba, Ondo and Borno States by the NCDC and partners
1.5.10. Offsite support provided by NCDC/partners in all affected States
1.5.11. NCDC and partners are providing onsite support in Ondo and Plateau State
1.5.12. States are enjoined to intensify surveillance and promote Infection, Prevention and Control (IPC) measures in health facilities.
2. MEASLES
2.1. In the reporting week, 209 suspected cases of Measles were reported from 29 States compared with 106 suspected cases reported from 25 States during the same period in 2016.
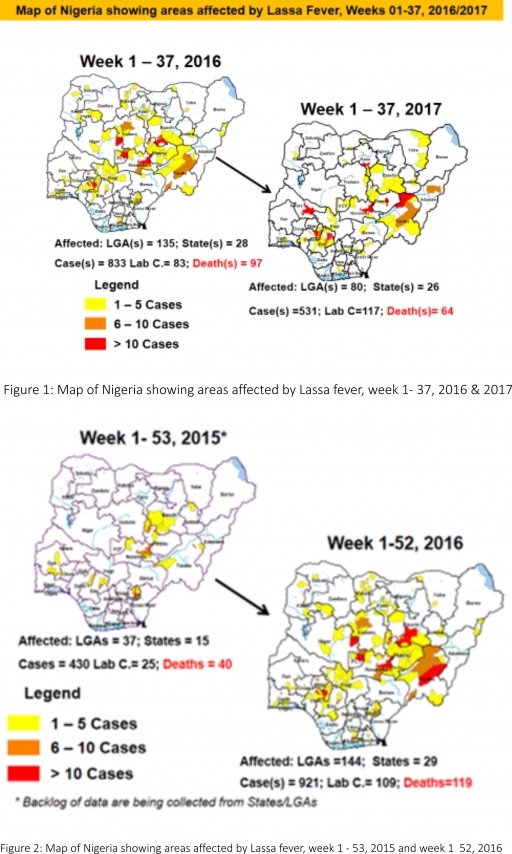
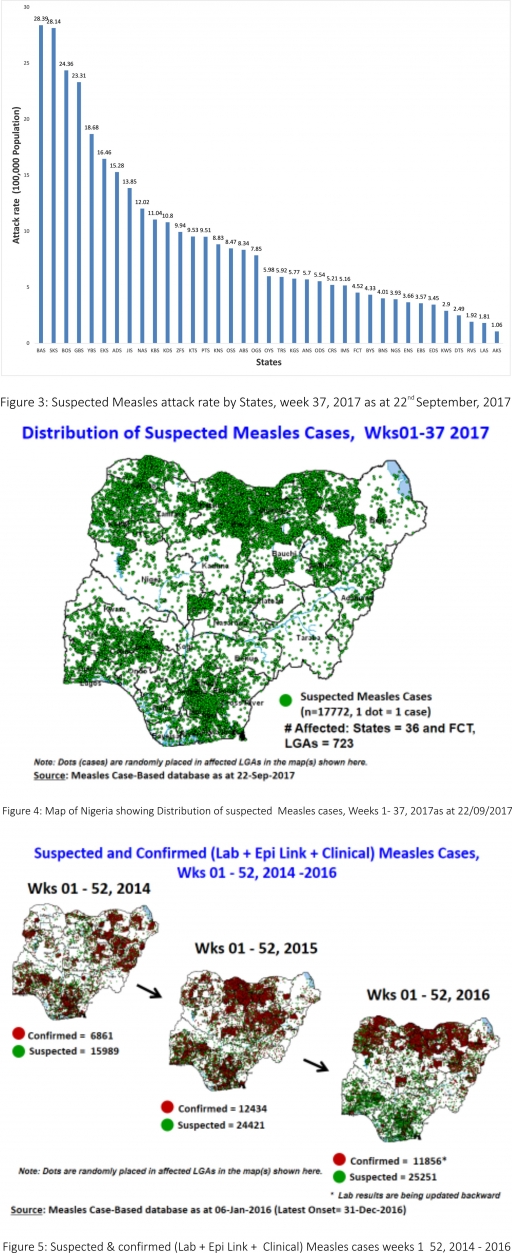
2.2. So far, 17,772 suspected Measles cases with 108 laboratory confirmed cases and 105 deaths (CFR, 0. 59%) have been reported in 2017 from 36 States and FCT (Figure 4) compared with 22,478 suspected cases and 99 deaths (CFR, 0.44%) from 36 States and FCT during the same period in 2016.
2.3. In 2016 (week 1 -52), 25,251 suspected Measles cases with 102 deaths (CFR, 0.40%) were reported from 36 States and FCT compared with 24,421 suspected cases with 127 deaths (CFR, 0.52%) during the same period in 2015 (Figure 5)
2.4. Response measures include immunization for all vaccine-preventable diseases in some selected/affected wards/LGAs during SIAs, as well as case management.
2.5. Scheduled Measles campaigns in the North East were conducted from 12th – 17th January 2017 in Adamawa, Borno and Yobe States (Phase I) and Phase II from 21st – 25th January 2017 in Borno State and 4th – 8th February 2017 in Yobe State
2.6. Measles Surveillance Evaluation and Establishment of the burden of Congenital Rubella Syndrome (CRS) in 12 selected States in the six geopolitical zones from the 17th -21st July 2017 conducted
2.6.1 Debrief meeting to review results and next steps from Measles evaluation conducted, held on the 15th of September 2017
2.7. Harmonisation of measles surveillance data with laboratory-confirmed cases
3. POLIOMYELITIS
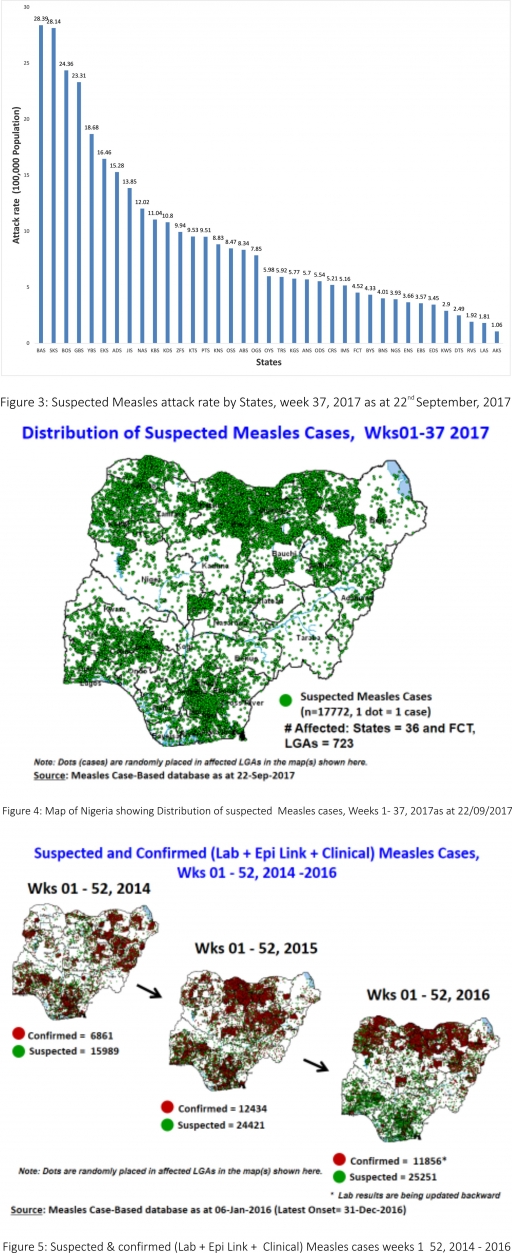
3.1. As at September 10th 2017, no new case of WPV was recorded
3.2. Three new cVDPV2, environmental derived and Polio compatible cases identified
3.2.1. In the reporting week, 224 cases of AFP were reported from 188 LGAs in 34 States and FCT
3.2.2. AFP Surveillance has been enhanced and outbreak response is on-going in Borno and other high-risk States
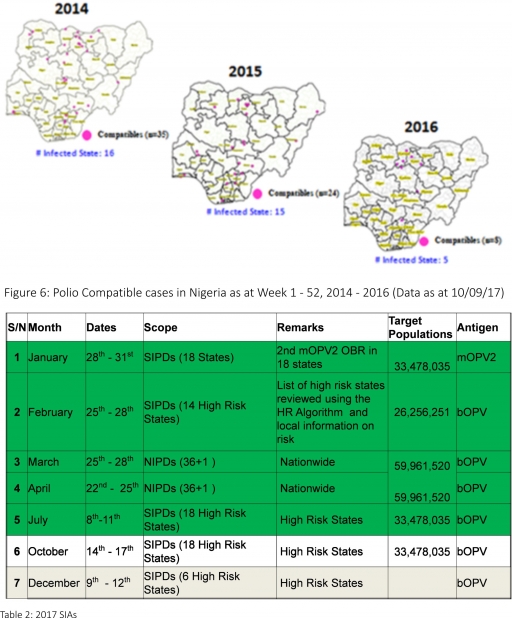
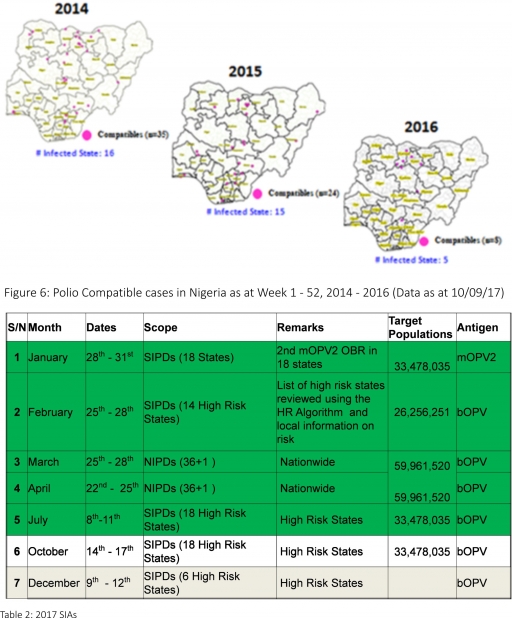
3.2.3. The 1st round of SIPDs in 2017 was conducted from 28th – 31st January 2017 in the 18 high-risk States. This was carried out using mOPV2 (2nd mOPV2 OBR). The schedule for other SIAs is as described in Table 2
3.2.4. The 2nd and 3rd round of SIPDs completed (25th-28th February and 8th – 11th July 2017) in 14 & 18 high-risk States using bOPV respectively.
3.2.5. The 1st and 2nd rounds of NIPDs completed (from 25th – 28th March 2017 and 22nd – 25th April 2017) nationwide respectively.
3.2.6. Between weeks 1 and 52 in 2016, four WPVs were isolated from Borno State compared to no WPV isolated during the same period in 2015.
3.3. No circulating Vaccine Derived Polio Virus type 2 (cVDPV2) was isolated in week 1 - 52, in both 2016 and 2015.
3.4. Between weeks 1 and 52, 2016 two (2) cVDPV2 were isolated in two LGAs (two States) while one (1) cVDPV2 was isolated from Kwali, FCT during the same period in 2015.
3.5. Six confirmed WPVs were isolated in 2014.
3.6. The SIAs were strengthened with the following events:
3.6.1. Immunisation for all vaccine-preventable diseases in some selected wards/LGAs.
3.6.2. Use of health camp facilities.
3.6.3. Field supportive supervision and monitoring.
3.6.4. Improved Enhanced Independent Monitoring (EIM) and Lots Quality Assessments (LQAs) in all Polio high-risk States.
3.6.5. High level of accountability framework
4. CHOLERA
4.1. 907 suspected cases of Cholera with one Laboratory confirmed and 26 deaths (CFR, 2.87%) were reported from eight LGAs (six States; Bauchi – 2, Borno – 842, Kaduna - 40 Kano – 5, Oyo – 1 and Zamfara - 17) in week 37 compared with seven suspected cases reported from two LGAs in Lagos State during the same period in 2016.
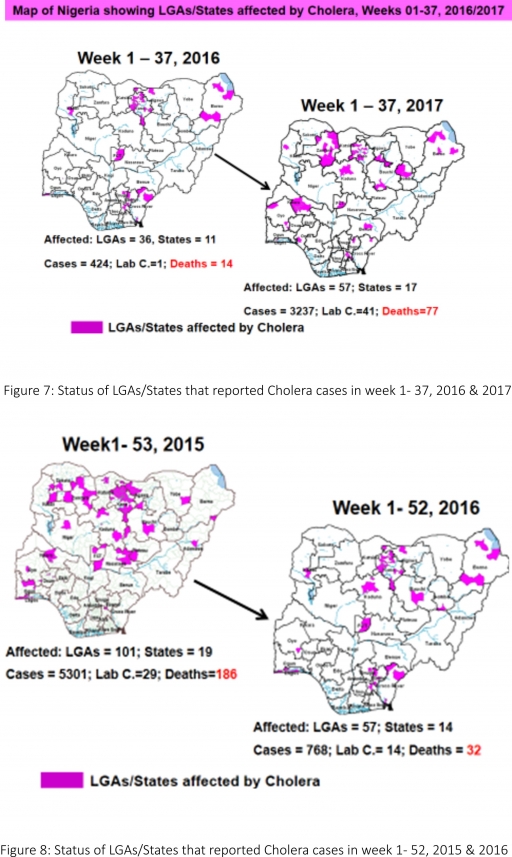
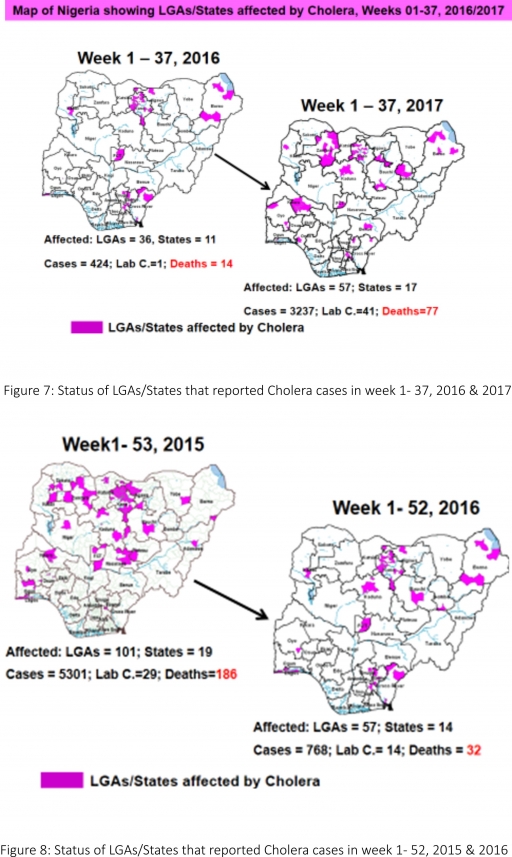
4.2. Between weeks 1 and 37 (2017), 3237 suspected Cholera cases with 41 laboratory confirmed and 77 deaths (CFR, 2.38%) from 57 LGAs (17 States) were reported compared with 424 suspected cases and 14 deaths (CFR, 3.30%) from 36 LGAs (11 States) during the same period in 2016 (Figure 7).
4.3. Between weeks 1 and 52 (2016), 768 suspected Cholera cases with 14 laboratory confirmed cases and 32 deaths (CFR, 4.17%) from 57 LGAs (14 States) were reported compared with 5,301 cases with 29 laboratory confirmed cases and 186 deaths (CFR, 3.51%) from 101 LGAs (18 States and FCT) during the same period in 2015 (Figure 8).
4.4. Cholera preparedness workshop held from 31st May – 1st June 2017 in Abuja to
develop Cholera preparedness plan as the season set in.
4.5. NCDC/partners provided onsite support in Kwara, Zamfara and Kebbi States.
4.6 NCDC/partners are providing onsite support in Borno State.
4.7. Cholera Preparedness Checklist sent to all States to assess their level of preparedness with recommendations for prevention of and response to an outbreak.
4.8. RDT procured by NCDC and WHO currently being prepositioned in affected States
4.9. States are enjoined to intensify surveillance, implement WASH activities and ensure early reporting.
5. CEREBROSPINAL MENINGITIS (CSM)
5.7. In the reporting week 37, two suspected Cerebrospinal Meningitis (CSM) cases were reported from two LGAs (two States) compared with 16 suspected cases from sixLGAs (five States) at the same period in 2016.
5.8. Between weeks 1 and 37 (2017), 9792 suspected CSM cases with 108 laboratory confirmed cases and 602 deaths (CFR, 6.15%) were recorded from 314 LGAs (33 States) compared with 655 suspected cases and 29 deaths (CFR, 4.43%) from 137 LGAs (28 States) during the same period in 2016 (Figure 9).
5.9. Between weeks 1 and 52, 2016, 831 suspected CSM cases with 43 laboratory confirmed cases and 33 deaths (CFR, 3.97%) were recorded from 154 LGAs (30 States and FCT) compared with 2,711 suspected cases and 131 deaths (CFR, 4.83%) from 170 LGAs (28 States and FCT) during the same period in 2015 (Figure 10)
5.10. Timeliness/completeness of CSM case-reporting from States to the National Level (2017 versus 2016): on average, 81.7% of the 26 endemic States sent CSM reports in a timely manner while 98.4% were complete in week 1 – 37, 2017 as against 85.6% timeliness and 99.9% completeness recorded within the same period in 2016
5.11. CSM preparedness checklist sent to 36 States and FCT ahead of 2017 meningitis season
5.12. Confirmed cases treated at identified treatment centres in affected States (Zamfara, Sokoto, Katsina, Kebbi, Niger, Kano, Yobe and Jigawa) and necessary supportive management also instituted
5.13. CSM National Emergency Operations Centre constituted at the Nigeria Centre for Disease Control
5.14. Onsite support provided to Zamfara, Sokoto, Katsina, Kebbi, Kano, Yobe and Niger States by NCDC and partners
5.15. Off-site support provided to other States
5.16. Intensive Surveillance in high-risk States and NCDC in communication with States reporting suspected cases.
5.17. Reactive vaccination completed in Zamfara, Sokoto and Yobe States
5.18. Medical teams were trained and deployed to support case management in Sokoto and Zamfara States completed (from Friday 5th - 26th May 2017).
5.19. Deployed mobile testing laboratory to Zamfara State to aid diagnosis
5.20. A Team was deployed by NCDC/WHO to support surveillance activities, laboratory data harmonization and monitoring of the implementation plan in Yobe state
5.21. Evaluation of the CSM outbreak response in Zamfara and Sokoto States is ongoing by NCDC and WHO
5.22. National CSM After-Action Review meeting conducted in Sokoto State from the 24th – 25th of July 2017.
5.23. NCDC attended the 14th Annual Meeting on Surveillance, Preparedness and Response to Meningitis Outbreaks in Africa, and 4th Annual MenAfriNet Partners’meeting held in Ouagadougou, Burkina Faso in preparation of 2017/2018 meningitis season from 12th to 15th September 2017.
5.24. Ongoing finalisation of the National CSM Guidelines

6. GUINEA WORM DISEASE
6.7. In the reporting week, no rumour report of Guinea Worm disease was received from any State.
6.8. Nigeria has celebrated eight consecutive years of zero reporting of Guinea worm disease in the country. The Country has been officially certified free of Dracunculiasis transmission by the International Commission for the Certification of Dracunculiasis Eradication (ICCDE).
(For further information, contact Nigeria Guinea Worm Eradication Program / Neglected Tropical Diseases Division, Public Health Department/Federal Ministry of Health)
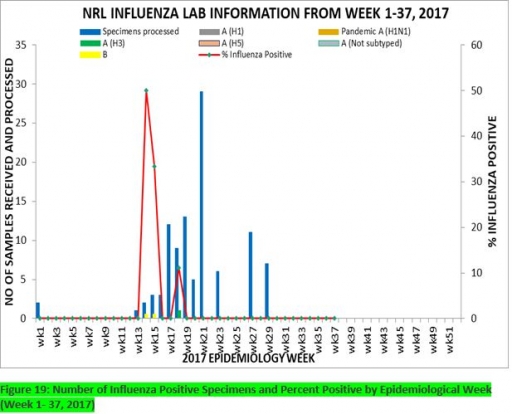
7. Update on national Influenza sentinel surveillance, Nigeria week 1 - 37, 2017
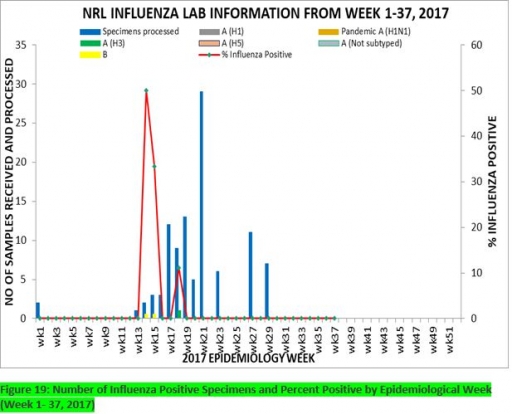
7.1. From week 1-37, a total of 103 cases were reported, of which 95 were Influenza-like-illness (ILI), 8 Severe Acute Respiratory Infection (SARI).
7.2 A total of 103 samples were received and all were processed. Of the processed samples, 95(92.2%) were ILI cases, 8(7.8%) were Severe Acute Respiratory Infection (SARI).
7.4. Of the 95 processed ILI samples, 1(1.05%) was positive for Influenza A; 2(2.1%) positive for Influenza B and 92(98.95%) were negative. Of the 8 processed SARI samples, none was positive for Influenza A and Influenza B.
7.5. Three (3.16%) of the processed 95 samples were positive for Influenza, with 1(33.3%) of these positive for Influenza A and 2(66.7%) positive for Influenza B. The subtypes A seasonal H3, 2009A/H1N1 and A/not subtyped account for (100%), 0(0.0%) and 0(0.0%) of the total influenza A positive sample respectively.
7.6. The percentage influenza positive was highest (50.0%) in week 14
7.7. In the reporting week 37, no samples were left unprocessed
FOR MORE INFORMATION CONTACT
Surveillance Unit:
Nigeria Centre for Disease Control
801 Ebitu Ukiwe Street, Jabi, Abuja, Nigeria.
[email protected]
www.ncdc.gov.ng/reports
0800-970000-10



 Toll Free Number: 6232
Toll Free Number: 6232 Whatsapp: +234 708 711 0839
Whatsapp: +234 708 711 0839 SMS Number: +234 809 955 5577
SMS Number: +234 809 955 5577 